Over 250 peer-reviewed scientific studies confirming that the spike protein (from virus or mRNA vaccine) is highly pathogenic on its own; most in vitro studies cited here used recombinant spike
proteins or spike proteins in pseudoviral vectors & produced pathological effects not reliant on the SARS-CoV2 viral machinery. Compiled by Dr. Martin Wucher, MSC Dent Sc (eq DDS), Erik Sass, et al.


Please retain these studies for your library and the issue is that if we are seeing the pathological nature of spike protein from the viral infection, the spike itself a toxic pathogen, then we can firmly extrapolate harms and death to the spike induced from the mRNA vaccine (and DNA viral vector platform).
Excellent scholarship by Dr. Martin Wucher, MSC Dent Sc (eq DDS), and Mr. Erik Sass
COVID-19 spike protein pathogenicity research library
Doi: 10.5281/zenodo.14269255
Over 250 high-quality studies (see TOXIC SHOT):
Last updated December 3, 2024. Corresponding author: eriksass@gmail.com
Originally part of the outer coat of the SARS-CoV2 virus, where it functions as a “key” to “unlock” (infect) cells, spike proteins are also produced in large amounts by the mRNA “vaccines,” triggering a short-lived immune response in the form of antibodies. However, a growing body of evidence has shown that the spike protein is harmful by itself, independent of the rest of the virus.
The following (I. Alphabetical List) collects over 250 peer-reviewed scientific studies confirming that the spike protein is highly pathogenic on its own; most in vitro studies cited here used recombinant spike proteins or spike proteins in pseudoviral vectors, and produced pathological effects not reliant on the SARS-CoV2 viral machinery.
The second section (II. Categories) organizes the research into broad categories including affected tissues and organ systems, mechanisms, and evidence from clinical pathology. Because these areas overlap, many articles appear more than once in the second section.
I. ALPHABETICAL LIST
1. Abdi A et al., “Biomed Interaction of SARS-CoV-2 with cardiomyocytes: Insight into the underlying molecular mechanisms of cardiac injury and pharmacotherapy,” Pharmacother. 2022, 146: 112518. doi: 10.1016/j.biopha.2021.112518
2. Aboudounya MM and RJ Heads, “COVID-19 and Toll-Like Receptor 4 (TLR4): SARS-CoV-2 May Bind and Activate TLR4 to Increase ACE2 Expression, Facilitating Entry and Causing Hyperinflammation,” Mediators Inflamm. 2021, 8874339. doi: https://doi.org/10.1155/2021/8874339
3. Acevedo-Whitehouse K and R Bruno, “Potential health risks of mRNA-based vaccine therapy: A hypothesis,” Med. Hypotheses 2023, 171: 111015. doi: https://doi.org/10.1016/j.mehy.2023.111015
4. Ahn WM et al., “SARS-CoV-2 Spike Protein Stimulates Macropinocytosis in Murine and Human Macrophages via PKC-NADPH Oxidase Signaling,” Antioxidants 2024, 13, 2: 175. doi: https://doi.org/10.3390/antiox13020175
5. Ait-Belkacem I et al., “SARS-CoV-2 spike protein induces a differential monocyte activation that may contribute to age bias in COVID-19 severity,” Sci. Rep. 2022, 12: 20824. doi: https://doi.org/10.1038/s41598-022-25259-2
6. Aksenova AY et al., “The increased amyloidogenicity of Spike RBD and pH-dependent binding to ACE2 may contribute to the transmissibility and pathogenic properties of SARS-CoV-2 omicron as suggested by in silico study,” Int. J. Mol. Sci. 2022, 23, 21: 13502. doi: https://doi.org/10.3390/ijms232113502
7. Al-Kuraishy HM et al., “Changes in the Blood Viscosity in Patients With SARS-CoV-2 Infection,” Front. Med. 2022, 9: 876017. doi: 10.3389/fmed.2022.876017
8. Al-Kuraishy HM et al., “Hemolytic anemia in COVID-19,” Ann. Hematol. 2022, 101: 1887–1895. doi: 10.1007/s00277-022-04907-7
9. Albornoz EA et al., “SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein,” Mol. Psychiatr. 2023, 28: 2878–2893. doi: https://doi.org/10.1038/s41380-022-01831-0
10. Almehdi AM et al., “SARS-CoV-2 Spike Protein: Pathogenesis, Vaccines, and Potential Therapies,” Infection 2021, 49, 5: 855–876. doi: https://doi.org/10.1007/s15010-021-01677-8
11. Angeli F et al., “COVID-19, vaccines and deficiency of ACE2 and other angiotensinases. Closing the loop on the ‘Spike effect’,” Eur J. Intern. Med. 2022, 103: 23–28. doi: 10.1016/j.ejim.2022.06.015
12. Angeli F et al., “The spike effect of acute respiratory syndrome coronavirus 2 and coronavirus disease 2019 vaccines on blood pressure,” Eur. J. Intern. Med. 2022, 109: 12-21. doi: 10.1016/j.ejim.2022.12.004
13. Ao Z et al., “SARS-CoV-2 Delta spike protein enhances the viral fusogenicity and inflammatory cytokine production,” iScience 2022, 25, 8: 104759. doi: 10.1016/j.isci.2022.104759
14. Appelbaum K et al., “SARS-CoV-2 spike-dependent platelet activation in COVID-19 vaccine-induced thrombocytopenia,” Blood Adv. 2022, 6: 2250–2253. doi: 10.1182/bloodadvances.2021005050
15. Arjsri P et al., “Hesperetin from root extract of Clerodendrum petasites S. Moore inhibits SARS-CoV-2 spike protein S1 subunit-induced Nlrp3 inflammasome in A549 lung cells via modulation of the Akt/Mapk/Ap-1 pathway,” Int. J. Mol. Sci. 2022, 23, 18: 10346. doi: https://doi.org/10.3390/ijms231810346
16. Asandei A et al., “Non-Receptor-Mediated Lipid Membrane Permeabilization by the SARS-CoV-2 Spike Protein S1 Subunit,” ACS Appl. Mater. Interfaces 2020, 12, 50: 55649–55658. doi: https://doi.org/10.1021/acsami.0c17044
17. Avolio E et al., “The SARS-CoV-2 Spike Protein Disrupts Human Cardiac Pericytes Function through CD147 Receptor-Mediated Signalling: A Potential Non-infective Mechanism of COVID-19 Microvascular Disease,” Clin. Sci. 2021, 135, 24: 2667–2689, doi: https://doi.org/10.1042/CS20210735
18. Baldari CT et al., “Emerging Roles of SARS-CoV-2 Spike-ACE2 in Immune Evasion and Pathogenesis,” Trends Immunol. 2023, 44, 6. doi: https://doi.org/10.1016/j.it.2023.04.001
19. Balzanelli MG et al., “The Role of SARS-CoV-2 Spike Protein in Long-term Damage of Tissues and Organs, the Underestimated Role of Retrotransposons and Stem Cells, a Working Hypothesis,” Endocr Metab Immune Disord Drug Targets 2025, 25, 2: 85-98. doi: 10.2174/0118715303283480240227113401
20. Barhoumi T et al., “SARS-CoV-2 coronavirus Spike protein-induced apoptosis, inflammatory, and oxidative stress responses in THP-1-like-macrophages: potential role of angiotensin-converting enzyme inhibitor (perindopril),” Front Immunol. 2021, 12: 728896. doi: https://doi.org/10.3389/fimmu.2021.728896
21. Barreda D et al., “SARS-CoV-2 Spike Protein and Its Receptor Binding Domain Promote a Proinflammatory Activation Profile on Human Dendritic Cells,” Cells 2021, 10, 12: 3279. doi: https://doi.org/10.3390/cells10123279
22. Baumeier C et al., “Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series,” Int. J. Mol. Sci. 2022, 23: 6940. doi: https://doi.org/10.3390/ijms23136940
23. Bellavite P et al., “Immune response and molecular mechanisms of cardiovascular adverse effects of spike proteins from SARS-coV-2 and mRNA vaccines,” Biomedicines 2023, 11, 2: 451. doi: https://doi.org/10.3390/biomedicines11020451
24. Bhargavan B and GD Kanmogne, “SARS-CoV-2 spike proteins and cell–cell communication inhibits TFPI and induces thrombogenic factors in human lung microvascular endothelial cells and neutrophils: implications for COVID-19 coagulopathy pathogenesis,” Int. J. Mol. Sci. 2022, 23, 18: 10436. doi: https://doi.org/10.3390/ijms231810436
25. Bhattacharyya S and JK Tobacman, “SARS-CoV-2 spike protein-ACE2 interaction increases carbohydrate sulfotransferases and reduces N-acetylgalactosamine-4-sulfatase by p38 MAPK,” Signal Transduct Target Ther 2024, 9, 39. doi: https://doi.org/10.1038/s41392-024-01741-3
26. Biancatelli RMLC et al., “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Kappa18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am. J. Physiol. Lung Cell. Mol. Physiol. 2021, 321, L477–L484. doi: https://doi.org/10.1152/ajplung.00223.2021
27. Biering SB et al., “SARS-CoV-2 Spike Triggers Barrier Dysfunction and Vascular Leak via Integrins and TGF-β Signaling,” Nat. Commun. 2022, 13: 7630. doi: https://doi.org/10.1038/s41467-022-34910-5
28. Bocquet-Garcon A, “Impact of the SARS-CoV-2 Spike Protein on the Innate Immune System: A Review,” Cureus 2024, 16, 3: e57008. doi: 10.7759/cureus.57008
29. Boretti A, “PQQ Supplementation and SARS-CoV-2 Spike Protein-Induced Heart Inflammation,” Nat. Prod. Commun. 2022, 17, 1934578×221080929. doi: https://doi.org/10.1177/1934578X221080929
30. Bortolotti D et al., “SARS-CoV-2 Spike 1 Protein Controls Natural Killer Cell Activation via the HLA-E/NKG2A Pathway,” Cells 2020, 9, 9: 1975. doi: https://doi.org/10.3390/cells9091975
31. Boschi C et al., “SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects,” Int. J. Biol. Macromol. 2022, 23, 24: 15480. doi: https://doi.org/10.3390/ijms232415480
32. Braga L et al., “Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia,” Nature 2021, 594: 88–93. doi: https://doi.org/10.1038/s41586-021-03491-6
33. Buoninfante A et al., “Myocarditis associated with COVID-19 vaccination,” npj Vaccines 2024, 122. doi: https://doi.org/10.1038/s41541-024-00893-1
34. Burkhardt A, “Pathology Conference: Vaccine-Induced Spike Protein Production in the Brain, Organs etc., now Proven,” Report24.news. 2022, https://report24.news/pathologie-konferenz-impfinduzierte-spike-produktion-in-gehirn-u-a-organen-nun-erwiesen/
35. Burnett FN et al., “SARS-CoV-2 Spike Protein Intensifies Cerebrovascular Complications in Diabetic hACE2 Mice through RAAS and TLR Signaling Activation,” Int. J. Mol. Sci. 2023, 24, 22: 16394. doi: https://doi.org/10.3390/ijms242216394
36. Buzhdygan TP et al., “The SARS-CoV-2 Spike Protein Alters Barrier Function in 2D Static and 3D Microfluidic in-Vitro Models of the Human Blood-Brain Barrier,” Neurobiol. Dis. 2020, 146, 105131. doi: https://doi.org/10.1016/j.nbd.2020.105131
37. Bye AP et al., “Aberrant glycosylation of anti-SARS-CoV-2 spike IgG is a prothrombotic stimulus for platelets,” Blood 2021, 138, 6: 1481–9. doi: https://doi.org/10.1182/blood.2021011871
38. Cao JB et al., “Mast cell degranulation-triggered by SARS-CoV-2 induces tracheal-bronchial epithelial inflammation and injury,” Virol. Sin. 2024, 39, 2: 309-318. doi: https://doi.org/10.1016/j.virs.2024.03.001
39. Cao S et al., “Spike Protein Fragments Promote Alzheimer’s Amyloidogenesis,” ACS Appl. Mater. Interfaces 2023, 15, 34: 40317-40329. doi: https://doi.org/10.1021/acsami.3c09815
40. Cao X et al., “Spike protein of SARS-CoV-2 activates macrophages and contributes to induction of acute lung inflammation in male mice,” FASEB J. 2021, 35, e21801. doi: https://doi.org/10.1096/fj.202002742RR
41. Cao X et al., “The SARS-CoV-2 spike protein induces long-term transcriptional perturbations of mitochondrial metabolic genes, causes cardiac fibrosis, and reduces myocardial contractile in obese mice,” Mol. Metab. 2023, 74, 101756. doi: https://doi.org/10.1016/j.molmet.2023.101756
42. Caohuy H et al., “Inflammation in the COVID-19 airway is due to inhibition of CFTR signaling by the SARS-CoV-2 spike protein,” Sci. Rep. 2024, 14: 16895. doi: https://doi.org/10.1038/s41598-024-66473-4
43. Carnevale R et al., “Toll-Like Receptor 4-Dependent Platelet-Related Thrombosis in SARS-CoV-2 Infection,” Circ. Res. 2023, 132, 3: 290– 305, doi: https://doi.org/10.1161/CIRCRESAHA.122.321541
44. Cattin‐Ortolá J et al., “Sequences in the cytoplasmic tail of SARS‐CoV‐2 Spike facilitate expression at the cell surface and syncytia formation,” Nat Commun 2021, 12, 1: 5333. doi: https://doi.org/10.1038/s41467-021-25589-1
45. Chang MH et al., “SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin,” Biomedicines 2024, 12, 6: 1223. doi: https://doi.org/10.3390/biomedicines12061223
46. Chaves JCS et al., “Differential Cytokine Responses of APOE3 and APOE4 Blood–brain Barrier Cell Types to SARS-CoV-2 Spike Proteins,” J. Neuroimmune Pharmacol. 2024, 19, 22. doi: https://doi.org/10.1007/s11481-024-10127-9
47. Cheng MH et al., “Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation,” Proc Natl Acad Sci 2020, 117: 25254–25262. doi: https://doi.org/10.1073/pnas.201072211
48. Chiok K et al., “Proinflammatory Responses in SARS-CoV-2 and Soluble Spike Glycoprotein S1 Subunit Activated Human Macrophages,” Viruses 2023, 15, 3: 754. doi: https://doi.org/10.3390/v15030754
49. Chittasupho C et al., “Inhibition of SARS-CoV-2-Induced NLRP3 Inflammasome-Mediated Lung Cell Inflammation by Triphala-Loaded Nanoparticle Targeting Spike Glycoprotein S1,” Pharmaceutics 2024, 16, 6: 751. https://doi.org/10.3390/pharmaceutics16060751
50. Chittasupho C et al., “Targeting spike glycoprotein S1 mediated by NLRP3 inflammasome machinery and the cytokine releases in A549 lung epithelial cells by nanocurcumin,” Pharmaceuticals (Basel) 2023, 16, 6: 862. doi: https://doi.org/10.3390/ph16060862
51. Choi JY et al., “SARS-CoV-2 spike S1 subunit protein-mediated increase of beta-secretase 1 (BACE1) impairs human brain vessel cells,” Biochem. Biophys. Res. Commun. 2022, 625, 20: 66-71. doi: https://doi.org/10.1016/j.bbrc.2022.07.113
52. Clemens DJ et al., “SARS-CoV-2 spike protein-mediated cardiomyocyte fusion may contribute to increased arrhythmic risk in COVID-19,” PLoS One 2023, 18, 3: e0282151. doi: https://doi.org/10.1371/journal.pone.0282151
53. Clough E et al., “Mitochondrial Dynamics in SARS-COV2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID,” Journal of Neuroimmune Pharmacology 2021, 16, 4: 770–784. doi: https://doi.org/10.1007/s11481-021-10015-6
54. Correa Y et al., “SARS-CoV-2 spike protein removes lipids from model membranes and interferes with the capacity of high-density lipoprotein to exchange lipids,” J. Colloid Interface Sci. 2021, 602: 732-739. doi: https://doi.org/10.1016/j.jcis.2021.06.056
55. Corpetti C et al., “Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line,” Phytother. Res. 2021, 35, 12: 6893–6903. doi: https://doi.org/10.1002/ptr.7302
56. Cory TJ et al., “Metformin Suppresses Monocyte Immunometabolic Activation by SARS-CoV-2 Spike Protein Subunit 1,” Front. Immunol. 2021, 12 (Sec. Cytokines and Soluble Mediators in Immunity): 733921. doi: https://doi.org/10.3389/fimmu.2021.733921
57. Cosentino M and Franca Marino, “Understanding the Pharmacology of COVID- 19 mRNA Vaccines: Playing Dice with the Spike?” Int. J. Mol. Sci. 2022, 23, 18: 10881. doi: https://doi.org/10.3390/ijms231810881
58. Cossenza LC et al., “Inhibitory effects of SARS-CoV-2 spike protein and BNT162b2 vaccine on erythropoietin-induced globin gene expression in erythroid precursor cells from patients with β-thalassemia,” Exp. Hematol. 2024, 129, 104128. doi: https://doi.org/10.1016/j.exphem.2023.11.002
59. Craddock V et al., “Persistent circulation of soluble and extracellular vesicle-linked Spike protein in individuals with postacute sequelae of COVID-19,” J Med. Virol. 2023, 95, 2: e28568. doi: https://doi.org/10.1002/jmv.28568
60. Das T et al., “N-glycosylation of the SARS-CoV-2 spike protein at Asn331 and Asn343 is involved in spike-ACE2 binding, virus entry, and regulation of IL-6,” Microbiol. Immunol. 2024, 68, 5: 165-178. doi: https://doi.org/10.1111/1348-0421.13121
61. De Michele M et al., “Evidence of SARS-CoV-2 Spike Protein on Retrieved Thrombi from COVID-19 Patients,” Journal of Hematology Oncology 2022, 15, 108. doi: https://doi.org/10.1186/s13045-022-01329-w
62. De Michele M et al., “Vaccine-induced immune thrombotic thrombocytopenia: a possible pathogenic role of ChAdOx1 nCoV-19 vaccine-encoded soluble SARS-CoV-2 spike protein,” Haematologica 2022, 107, 7: 1687–92. doi: https://doi.org/10.3324/haematol.2021.280180
63. De Sousa PMB et al., “Fatal Myocarditis following COVID-19 mRNA Immunization: A Case Report and Differential Diagnosis Review,” Vaccines 2024, 12, 2: 194. doi: https://doi.org/10.3390/vaccines12020194
64. Del Re A et al., “Intranasal delivery of PEA-producing Lactobacillus paracasei F19 alleviates SARS-CoV-2 spike protein-induced lung injury in mice,” Transl. Med. Commun. 2024, 9, 9. doi: https://doi.org/10.1186/s41231-024-00167-x
65. Del Re A et al., “Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages,” Metabolites 2021, 11, 9: 592. doi: https://doi.org/10.3390/metabo11090592
66. DeOre BJ et al., “SARS-CoV-2 Spike Protein Disrupts Blood-Brain Barrier Integrity via RhoA Activation,” J Neuroimmune Pharmacol. 2021, 16, 4: 722-728. doi: https://doi.org/10.1007/s11481-021-10029-0
67. Devaux CA and L. Camoin-Jau, “Molecular mimicry of the viral spike in the SARS-CoV-2 vaccine possibly triggers transient dysregulation of ACE2, leading to vascular and coagulation dysfunction similar to SARS-CoV-2 infection,” Viruses 2023, 15, 5: 1045. doi: https://doi.org/10.3390/v15051045
68. Dissook S et al., “Luteolin-rich fraction from Perilla frutescens seed meal inhibits spike glycoprotein S1 of SARS-CoV-2-induced NLRP3 inflammasome lung cell inflammation via regulation of JAK1/STAT3 pathway: A potential anti-inflammatory compound against inflammation-induced long-COVID,” Front. Med. 2023, 9: 1072056. doi: https://doi.org/10.3389/fmed.2022.1072056
69. Duarte C, “Age-dependent effects of the recombinant spike protein/SARS-CoV-2 on the M-CSF- and IL-34-differentiated macrophages in vitro,” Biochem. Biophys. Res. Commun. 2021, 546: 97–102. doi: https://doi.org/10.1016/j.bbrc.2021.01.104
70. Erdogan MA, “Prenatal SARS-CoV-2 Spike Protein Exposure Induces Autism-Like Neurobehavioral Changes in Male Neonatal Rats,” J Neuroimmune Pharmacol. 2023, 18, 4 :573-591. doi: 10.1007/s11481-023-10089-4
71. Fajloun Z et al., “SARS-CoV-2 or Vaccinal Spike Protein can Induce Mast Cell Activation Syndrome (MCAS),” Infect Disord Drug Targets, 2025, 25, 1: e300424229561. doi: 10.2174/0118715265319896240427045026
72. Ferrer MD et al., “Nitrite Attenuates the In Vitro Inflammatory Response of Immune Cells to the SARS-CoV-2 S Protein without Interfering in the Antioxidant Enzyme Activation,” Int. J. Mol. Sci. 2024, 25, 5: 3001. https://doi.org/10.3390/ijms25053001
73. Fontes-Dantas FL, “SARS-CoV-2 Spike Protein Induces TLR4-Mediated Long- Term Cognitive Dysfunction Recapitulating Post-COVID-19 Syndrome in Mice,” Cell Reports 2023, 42, 3: 112189. doi: https://doi.org/10.1016/j.celrep.2023.112189
74. Forsyth CB et al., “The SARS-CoV-2 S1 spike protein promotes MAPK and NF-kB activation in human lung cells and inflammatory cytokine production in human lung and intestinal epithelial cells,” Microorganisms 2022, 10, 10: 1996. doi: https://doi.org/10.3390/microorganisms10101996
75. Forte E, “Circulating spike protein may contribute to myocarditis after COVID-19 vaccination,” Nat. Cardiovasc. Res. 2023, 2: 100. doi: https://doi.org/10.1038/s44161-023-00222-0
76. Frank MG et al., “SARS-CoV-2 S1 subunit produces a protracted priming of the neuroinflammatory, physiological, and behavioral responses to a remote immune challenge: A role for corticosteroids,” Brain Behav. Immun. 2024, 121: 87-103. doi: https://doi.org/10.1016/j.bbi.2024.07.034
77. Frank MG et al., “SARS-CoV-2 Spike S1 Subunit Induces Neuroinflammatory, Microglial and Behavioral Sickness Responses: Evidence of PAMP-Like Properties,” Brain Behav. Immun. 2022, 100: 267277. doi: https://doi.org/10.1016/j.bbi.2021.12.007
78. Freeborn J, “Misfolded Spike Protein Could Explain Complicated COVID-19 Symptoms,” Medical News Today, May 26, 2022, https://www.medicalnewstoday.com/articles/misfolded-spike-protein-could-explain-complicated-covid-19-symptoms
79. Freitas RS et al., “SARS-CoV-2 Spike antagonizes innate antiviral immunity by targeting interferon regulatory factor 3,” Front Cell Infect Microbiol. 2021, 11: 789462. doi: https://doi.org/10.3389/fcimb.2021.789462
80. Frühbeck G et al., “FNDC4 and FNDC5 reduce SARS-CoV-2 entry points and spike glycoprotein S1-induced pyroptosis, apoptosis, and necroptosis in human adipocytes,” Cell Mol Immunol. 2021, 18, 10: 2457–9. doi: https://doi.org/10.1038/s41423-021-00762-0
81. Gamblicher T et al., “SARS‐CoV‐2 spike protein is present in both endothelial and eccrine cells of a chilblain‐like skin lesion,” J Eur Acad Dermatol Venereol. 2020, 1, 10: e187-e189. doi: https://doi.org/10.1111/jdv.16970
82. Gao X et al., “Spike-Mediated ACE2 Down-Regulation Was Involved in the Pathogenesis of SARS-CoV-2 Infection,” Journal of Infection 2022, 85, 4: 418–427, doi: 10.1016/j.jinf.2022.06.030
83. Gasparello J et al., “Sulforaphane inhibits the expression of interleukin-6 and interleukin-8 induced in bronchial epithelial IB3-1 cells by exposure to the SARS-CoV-2 Spike protein,” Phytomedicine 2021, 87: 153583. doi: https://doi.org/10.1016/j.phymed.2021.153583
84. Gawaz A et al., “SARS-CoV-2–Induced Vasculitic Skin Lesions Are Associated with Massive Spike Protein Depositions in Autophagosomes,” J Invest Dermatol. 2024, 144, 2: 369-377.e4. doi: https://doi.org/10.1016/j.jid.2023.07.018
85. Ghazanfari D et al., “Mechanistic insights into SARS-CoV-2 spike protein induction of the chemokine CXCL10,” Sci. Rep. 2024, 14: 11179. doi: https://doi.org/10.1038/s41598-024-61906-6
86. Golob-Schwarzl N et al., “SARS-CoV-2 spike protein functionally interacts with primary human conjunctival epithelial cells to induce a pro-inflammatory response,” Eye 2022, 36: 2353–5. doi: https://doi.org/10.1038/s41433-022-02066-7
87. Gracie NP et al., “Cellular signalling by SARS-CoV-2 spike protein,” Microbiology Australia 2024, 45, 1: 13-17. doi: https://doi.org/10.1071/MA24005
88. Greenberger JS et al., “SARS-CoV-2 Spike Protein Induces Oxidative Stress and Senescence in Mouse and Human Lung,” In Vivo 2024, 38, 4: 1546-1556; doi: https://doi.org/10.21873/invivo.13605
89. Grishma K and Das Sarma, “The Role of Coronavirus Spike Protein in Inducing Optic Neuritis in Mice: Parallels to the SARS-CoV-2 Virus,” J Neuroophthalmol 2024, 44, 3: 319-329. Doi: 10.1097/WNO.0000000000002234
90. Grobbelaar LM et al., “SARS-CoV-2 Spike Protein S1 Induces Fibrin(ogen) Resistant to Fibrinolysis: Implications for Microclot Formation in COVID-19,” Biosicence Reports 2021, 41, 8: BSR20210611. doi: https://doi.org/10.1042/BSR20210611
91. Gu T et al., “Cytokine Signature Induced by SARS-CoV-2 Spike Protein in a Mouse Model,” Front. Immunol. 2021 (Sec. Inflammation). doi: https://doi.org/10.3389/fimmu.2020.621441
92. Guo X et al., “Regulation of proinflammatory molecules and tissue factor by SARS-CoV-2 spike protein in human placental cells: implications for SARS-CoV-2 pathogenesis in pregnant women,” Front Immunol 2022, 13: 876555–876555. https://doi.org/10.3389/fimmu.2022.876555
93. Guo Y and V Kanamarlapudi, “Molecular Analysis of SARS-CoV-2 Spike Protein-Induced Endothelial Cell Permeability and vWF Secretion,” Int. J. Mol. Sci. 2023, 24, 6: 5664. https://doi.org/10.3390/ijms24065664
94. Gussow AB et al., “Genomic Determinants of Pathogenicity in SARS-CoV-2 and Other Human Coronaviruses,” PNAS 2020, 117, 26: 15193–15199. doi: https://doi.org/10.1073/pnas.2008176117
95. Halma MTJ et al., “Exploring autophagy in treating SARS-CoV-2 spike protein-related pathology,” Endocrinol Metab (EnM) 2024, 14: 100163. doi: https://doi.org/10.1016/j.endmts.2024.100163
96. Halma MTJ et al., “Strategies for the Management of Spike Protein-Related Pathology,” Microorganisms 2023, 11, 5: 1308, doi: https://doi.org/10.3390/microorganisms11051308
97. Heath SP et al., “SARS-CoV-2 Spike Protein Exacerbates Thromboembolic Cerebrovascular Complications in Humanized ACE2 Mouse Model,” Transl Stroke Res. 2024. doi: https://doi.org/10.1007/s12975-024-01301-5
98. Heil M, “Self-DNA driven inflammation in COVID-19 and after mRNA-based vaccination: lessons for non-COVID-19 pathologies,” Front. Immunol., 2023, 14. doi: https://doi.org/10.3389/fimmu.2023.1259879
99. Huang X et al., “Sars-Cov-2 Spike Protein-Induced Damage of hiPSC-Derived Cardiomyocytes,” Adv. Biol. 2022, 6, 7: e2101327. doi: https://doi.org/10.1002/adbi.202101327
100. Hulscher N et al., “Autopsy findings in cases of fatal COVID-19 vaccine-induced myocarditis,” ESC Heart Failure 2024. doi: https://doi.org/10.1002/ehf2.14680
101. Huynh TV et al., “Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19,” Cells 2023, 12, 877. doi: https://doi.org/10.3390/cells12060877
102. Huynh TV et al., “Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling,” Cells 2024, 13, 16: 1331: doi: https://doi.org/10.3390/cells13161331
103. Iba T and JH Levy, “The roles of platelets in COVID-19-associated coagulopathy and vaccine-induced immune thrombotic thrombocytopenia,” Trends Cardiovasc Med. 2022, 32, 1: 1-9. doi: https://doi.org/10.1016/j.tcm.2021.08.012
104. Idrees D and Vijay Kumar, “SARS-CoV-2 Spike Protein Interactions with Amyloidogenic Proteins: Potential Clues to Neurodegeneration,” Biochem Biophys Res Commun. 2021, 554 : 94–98, doi: https://doi.org/10.1016/j.bbrc.2021.03.100
105. Imig JD, “SARS-CoV-2 spike protein causes cardiovascular disease independent of viral infection,” Clin Sci (Lond) 2022, 136, 6: 431–434. doi: https://doi.org/10.1042/CS20220028
106. Jana S et al., “Cell-free hemoglobin does not attenuate the effects of SARS-CoV-2 spike protein S1 subunit in pulmonary endothelial cells,” Int. J. Mol. Sci. 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
107. Jiang Q et al., “SARS-CoV-2 spike S1 protein induces microglial NLRP3-dependent neuroinflammation and cognitive impairment in mice,” Exp. Neurol. 2025, 383: 115020. doi: https://doi.org/10.1016/j.expneurol.2024.115020
108. Johnson EL et al., “The S1 spike protein of SARS-CoV-2 upregulates the ERK/MAPK signaling pathway in DC-SIGN-expressing THP-1 cells,” Cell Stress Chaperones 2024, 29, 2: 227-234. doi: https://doi.org/10.1016/j.cstres.2024.03.002
109. Jugler C et al, “SARS-CoV-2 Spike Protein-Induced Interleukin 6 Signaling Is Blocked by a Plant-Produced Anti-Interleukin 6 Receptor Monoclonal Antibody,” Vaccines 2021, 9, 11: 1365. https://doi.org/10.3390/vaccines9111365
110. Kammala AK et al., “In vitro mRNA-S maternal vaccination induced altered immune regulation at the maternal-fetal interface,” Am. J. Reprod. Immunol. 2024, 91, 5: e13861. doi:
https://doi.org/10.1111/aji.13861
111. Karwaciak I et al., “Nucleocapsid and Spike Proteins of the Coronavirus Sars-Cov-2 Induce Il6 in Monocytes and Macrophages—Potential Implications for Cytokine Storm Syndrome,” Vaccines 2021, 9(1), 54: 1–10. doi: https://doi.org/10.3390/vaccines9010054
112. Kato Y et al., “TRPC3-Nox2 Protein Complex Formation Increases the Risk of SARS-CoV-2 Spike Protein-Induced Cardiomyocyte Dysfunction through ACE2 Upregulation,” Int. J. Mol. Sci. 2023, 24, 1: 102. doi: https://doi.org/10.3390/ijms24010102
113. Ken W et al., “Low dose radiation therapy attenuates ACE2 depression and inflammatory cytokines induction by COVID-19 viral spike protein in human bronchial epithelial cells,” Int J Radiat Biol. 2022, 98, 10: 1532-1541. doi: https://doi.org/10.1080/09553002.2022.2055806
114. Khaddaj-Mallat R et al., “SARS-CoV-2 deregulates the vascular and immune functions of brain pericytes via Spike protein,” Neurobiol. Dis. 2021, 161, 105561. doi: https://doi.org/10.1016/j.nbd.2021.105561
115. Khan S et al., “SARS-CoV-2 Spike Protein Induces Inflammation via TLR2-Dependent Activation of the NF-κB Pathway,” eLife 2021, 10: e68563. doi: https://doi.org/10.7554/elife.68563
116. Kim ES et al., “Spike Proteins of SARS-CoV-2 Induce Pathological Changes in Molecular Delivery and Metabolic Function in the Brain Endothelial Cells,” Viruses, 2021, 13, 10. doi: https://doi.org/10.3390/v13102021
117. Kim MJ et al., “The SARS‐CoV‐2 spike protein induces lung cancer migration and invasion in a TLR2‐dependent manner,” Cancer Commun (London), 2023, 44, 2: 273–277. doi: https://doi.org/10.1002/cac2.12485
118. Kim SY et al., “Characterization of heparin and severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) spike glycoprotein binding interactions,” Antivir Res. 2020, 181: 104873. doi: https://doi.org/10.1016/j.antiviral.2020.104873
119. Kircheis R, “Coagulopathies after Vaccination against SARS-CoV-2 May Be Derived from a Combined Effect of SARS-CoV-2 Spike Protein and Adenovirus Vector-Triggered Signaling Pathways,” Int. J. Mol. Sci. 2021, 22, 19: 10791. https://doi.org/10.3390/ijms221910791
120. Kircheis R and O Planz, “Could a Lower Toll-like Receptor (TLR) and NF-κB Activation Due to a Changed Charge Distribution in the Spike Protein Be the Reason for the Lower Pathogenicity of Omicron?” Int. J. Mol. Sci. 2022, 23, 11: 5966. doi: https://doi.org/10.3390/ijms23115966
121. Ko CJ et al., “Discordant anti-SARS-CoV-2 spike protein and RNA staining in cutaneous perniotic lesions suggests endothelial deposition of cleaved spike protein,” J. Cutan Pathol 2021, 48, 1: 47–52. doi: https://doi.org/10.1111/cup.13866
122. Kowarz E et al., “Vaccine-induced COVID-19 mimicry syndrome,” eLife 2022, 11: e74974. doi: https://doi.org/10.7554/eLife.74974
123. Kucia M et al., “An evidence that SARS-Cov-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner,” Leukemia 2021, 35: 3026-3029. doi: https://doi.org/10.1038/s41375-021-01332-z
124. Kuhn CC et al., “Direct Cryo-ET observation of platelet deformation induced by SARS-CoV-2 spike protein,” Nat. Commun. (2023) 14, 620. doi: https://doi.org/10.1038/s41467-023-36279-5
125. Kulkoviene G et al., “Differential Mitochondrial, Oxidative Stress and Inflammatory Responses to SARS-CoV-2 Spike Protein Receptor Binding Domain in Human Lung Microvascular, Coronary Artery Endothelial and Bronchial Epithelial Cells,” Int. J. Mol. Sci. 2024, 25, 6: 3188. doi: https://doi.org/10.3390/ijms25063188
126. Kumar N et al., “SARS-CoV-2 spike protein S1-mediated endothelial injury and pro-inflammatory state Is amplified by dihydrotestosterone and prevented by mineralocorticoid antagonism,” Viruses 2021, 13, 11: 2209. Doi: https://doi.org/10.3390/v13112209
127. Kyriakopoulos AM et al., “Mitogen Activated Protein Kinase (MAPK) Activation, p53, and Autophagy Inhibition Characterize the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Protein Induced Neurotoxicity,” Cureus 2022, 14, 12: e32361. doi: 10.7759/cureus.32361
128. Lazebnik Y, “Cell fusion as a link between the SARS-CoV-2 spike protein, COVID-19 complications, and vaccine side effects,” Oncotarget 2021, 12, 25: 2476-2488. doi: https://doi.org/10.18632/oncotarget.28088
129. Lehmann KJ, “Impact of SARS-CoV-2 Spikes on Safety of Spike-Based COVID-19 Vaccinations,” Immunome Res. 2024, 20, 2: 1000267. doi: 10.35248/1745-7580.24.20.267
130. Lehmann KJ, “SARS-CoV-2-Spike Interactions with the Renin-Angiotensin-Aldosterone System – Consequences of Adverse Reactions of Vaccination,” J Biol Today’s World 2023, 12/4: 001-013. https://doi.org/10.31219/osf.io/27g5h
131. Lehmann KJ, “Suspected Causes of the Specific Intolerance Profile of Spike-Based Covid-19 Vaccines,” Med. Res. Arch 2024, 12, 9. doi: 10.18103/mra.v12i9.5704
132. Lei Y et al., “SARS-CoV-2 Spike Protein Impairs Endothelial Function via Downregulation of ACE 2,” Circ. Res. 2021, 128, 9: 1323–1326. doi: https://doi.org/10.1161/CIRCRESAHA.121.318902
133. Lesgard JF et al., “Toxicity of SARS-CoV-2 Spike Protein from the Virus and Produced from COVID-19 mRNA or Adenoviral DNA Vaccines,” Arch Microbiol Immun 2023, 7, 3: 121-138. doi: 10.26502/ami.936500110
134. Letarov AV et al., “Free SARS-CoV-2 Spike Protein S1 Particles May Play a Role in the Pathogenesis of COVID-19 Infection,” Biochemistry (Moscow) 2021, 86: 257–261. doi: https://doi.org/10.1134/S0006297921030032
135. Li F et al., “SARS-CoV-2 Spike Promotes Inflammation and Apoptosis Through Autophagy by ROS-Suppressed PI3K/AKT/mTOR Signaling,” Biochim Biophys Acta BBA – Mol Basis Dis 2021, 1867: 166260. doi: https://doi.org/10.1016/j.bbadis.2021.166260
136. Li K et al., “SARS-CoV-2 Spike protein promotes vWF secretion and thrombosis via endothelial cytoskeleton-associated protein 4 (CKAP4),” Signal Transduct Targ Ther 2022, 7, 332. doi: https://doi.org/10.1038/s41392-022-01183-9
137. Li T et al., “Platelets Mediate Inflammatory Monocyte Activation by SARS-CoV-2 Spike Protein,” J. Clin. Invest. 2022, 132, 4: e150101. doi: 10.1172/JCI150101
138. Li Z et al., “SARS-CoV-2 pathogenesis in the gastrointestinal tract mediated by Spike-induced intestinal inflammation,” Precis. Clin. Med. 2024, 7, 1: pbad034. doi: https://doi.org/10.1093/pcmedi/pbad034
139. Liang S et al., “SARS-CoV-2 spike protein induces IL-18-mediated cardiopulmonary inflammation via reduced mitophagy,” Signal Transduct Target Ther 2023, 8, 103. doi: https://doi.org/10.1038/s41392-023-01368-w
140. Lin Z, “More than a key—the pathological roles of SARS-CoV-2 spike protein in COVID-19 related cardiac injury,” Sports Med Health Sci 2023, 6, 3: 209-220. doi: https://doi.org/10.1016/j.smhs.2023.03.004
141. Liu T et al., “RS-5645 attenuates inflammatory cytokine storm induced by SARS-CoV-2 spike protein and LPS by modulating pulmonary microbiota,” Int J Biol Sci. 2021, 17, 13: 3305–3319. doi: 10.7150/ijbs.63329
142. Liu X et al., “SARS-CoV-2 spike protein-induced cell fusion activates the cGAS-STING pathway and the interferon response,” Sci Signal. 2022, 15, 729: eabg8744. doi: 10.1126/scisignal.abg8744
143. Loh D, “The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding,” Melatonin Research 2020, 3, 3: 380-416. doi: https://doi.org/10.32794/mr11250069
144. Loh JT et al., “Dok3 restrains neutrophil production of calprotectin during TLR4 sensing of SARS-CoV-2 spike protein,” Front. Immunol. 2022, 13 (Sec. Molecular Innate Immunity). doi: https://doi.org/10.3389/fimmu.2022.996637
145. Lu J and PD Sun, “High affinity binding of SARS-CoV-2 spike protein enhances ACE2 carboxypeptidase activity,” J. Biol. Chem 2020, 295, 52: p18579-18588. doi: 10.1074/jbc.RA120.015303
146. Luchini A et al., “Lipid bilayer degradation induced by SARS-CoV-2 spike protein as revealed by neutron reflectometry,” Sci. Rep. 2021, 11: 14867. doi: https://doi.org/10.1038/s41598-021-93996-x
147. Luo Y et al., “SARS-Cov-2 spike induces intestinal barrier dysfunction through the interaction between CEACAM5 and Galectin-9,” Front. Immunol., 2024, 15. doi: https://doi.org/10.3389/fimmu.2024.1303356
148. Lykhmus O et al., “Immunization with 674–685 fragment of SARS-Cov-2 spike protein induces neuroinflammation and impairs episodic memory of mice,” Biochem. Biophys. Res. Commun. 2022, 622: 57–63. doi: https://doi.org/10.1016/j.bbrc.2022.07.016
149. Ma G et al., “SARS-CoV-2 Spike protein S2 subunit modulates γ-secretase and enhances amyloid-β production in COVID-19 neuropathy,” Cell Discov 2022, 8, 99. doi: https://doi.org/10.1038/s41421-022-00458-3
150. Maeda Y et al., “Differential Ability of Spike Protein of SARS-CoV-2 Variants to Downregulate ACE2,” Int. J. Mol. Sci. 2024, 25, 2: 1353. doi: https://doi.org/10.3390/ijms25021353
151. Magen E et al., “Clinical and Molecular Characterization of a Rare Case of BNT162b2 mRNA COVID-19 Vaccine-Associated Myositis,” Vaccines 2022, 10: 1135. doi: https://doi.org/10.3390/vaccines10071135
152. Magro N et al., “Disruption of the blood-brain barrier is correlated with spike endocytosis by ACE2 + endothelia in the CNS microvasculature in fatal COVID-19. Scientific commentary on ‘Detection of blood-brain barrier disruption in brains of patients with COVID-19, but no evidence of brain penetration by SARS-CoV-2’,” Acta Neuropathol. 2024, 147, 1: 47. doi: https://doi.org/10.1007/s00401-023-02681-y
153. Marrone L et al., “Tirofiban prevents the effects of SARS-CoV-2 spike protein on macrophage activation and endothelial cell death,” Heliyon 2024, 10, 15: e35341. doi: 10.1016/j.heliyon.2024.e35341
154. Martinez-Marmol R et al., “SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity,” Sci. Adv. 2023, 9, 23. doi: 10.1126/sciadv.adg2248
155. Matsuzawa Y et al., “Impact of Renin–Angiotensin–Aldosterone System Inhibitors on COVID-19,” Hypertens Res. 2022, 45, 7: 1147–1153. doi: https://doi.org/10.1038/s41440-022-00922-3
156. Maugeri N et al., “Unconventional CD147-Dependent Platelet Activation Elicited by SARS-CoV-2 in COVID-19,” J. Thromb. Haemost. 2021, 20, 2: 434–448. doi: https://doi.org/10.1111/jth.15575
157. Mercado-Gómez M et al., “The spike of SARS-CoV-2 promotes metabolic rewiring in hepatocytes,” Commun. Biol. 2022, 5, 827. doi: https://doi.org/10.1038/s42003-022-03789-9
158. Meyer K et al., “SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells,” J. Virol. 2021, 95, e0079421. doi: https://doi.org/10.1128/jvi.00794-21
159. Miller GM et al., “SARS-CoV-2 and SARS-CoV-2 Spike protein S1 subunit Trigger Proinflammatory Response in Macrophages in the Absence of Productive Infection,” J. Immunol. 2023, 210 (1_Supplement): 71.30. doi: https://doi.org/10.4049/jimmunol.210.Supp.71.30
160. Mishra R and AC Banerjea, “SARS-CoV-2 Spike targets USP33-IRF9 axis via exosomal miR-148a to activate human microglia,” Front. Immunol. 2021, 12: 656700. doi: https://doi.org/10.3389/fimmu.2021.656700
161. Mörz M, “A Case Report: Multifocal Necrotizing Encephalitis and Myocarditis after BNT162b2 mRNA Vaccination against COVID-19,” Vaccines 2022, 10, 10: 1651. doi: https://doi.org/10.3390/vaccines10101651
162. Moutal A et al., “SARS-CoV-2 Spike protein co-opts VEGF-A/Neuropilin-1 receptor signaling to induce analgesia,” Pain 2020, 162, 1: 243–252. doi: 10.1097/j.pain.0000000000002097
163. Munavilli GG et al., “COVID-19/SARS-CoV-2 virus spike protein-related delayed inflammatory reaction to hyaluronic acid dermal fillers: a challenging clinical conundrum in diagnosis and treatment,” Arch. Dermatol. Res. 2022, 314: 1-15. doi: https://doi.org/10.1007/s00403-021-02190-6
164. Nahalka J, “1-L Transcription of SARS-CoV-2 Spike Protein S1 Subunit,” Int. J. Mol. Sci. 2024, 25, 8: 4440. doi: https://doi.org/10.3390/ijms25084440
165. Nascimento RR et al., “SARS-CoV-2 Spike protein triggers gut impairment since mucosal barrier to innermost layers: From basic science to clinical relevance,” Mucosal Immunol. 2024, 17, 4: 565-583. doi: https://doi.org/10.1016/j.mucimm.2024.03.00
166. Nguyen V, “The Spike Protein of SARS-CoV-2 Impairs Lipid Metabolism and Increases Susceptibility to Lipotoxicity: Implication for a Role of Nrf2,” Cells 2022, 11, 12: 1916. doi: https://doi.org/10.3390/cells11121916
167. Niu C et al., “SARS-CoV-2 spike protein induces the cytokine release syndrome by stimulating T cells to produce more IL-2,” Front. Immunol. 2024, 15: 1444643. doi: https://doi.org/10.3389/fimmu.2024.1444643
168. Norris B et al., “Evaluation of Glutathione in Spike Protein of SARS-CoV-2 Induced Immunothrombosis and Cytokine Dysregulation,” Antioxidants 2024, 13, 3: 271. doi: https://doi.org/10.3390/antiox13030271
169. Nunez-Castilla J et al., “Potential autoimmunity resulting from molecular mimicry between SARS-CoV-2 spike and human proteins,” Viruses 2022, 14, 7: 1415. doi: https://doi.org/10.3390/v14071415
170. Nuovo JG et al., “Endothelial Cell Damage Is the Central Part of COVID-19 and a Mouse Model Induced by Injection of the S1 Subunit of the Spike Protein,” Ann. Diagn. Pathol. 2021, 51, 151682. doi: https://doi.org/10.1016/j.anndiagpath.2020.151682
171. Nyström S, “Amyloidogenesis of SARS-CoV-2 Spike Protein,” J. Am. Chem. Soc. 2022, 144, 8945–8950. doi: https://doi.org/10.1021/jacs.2c03925
172. Oh J et al., “SARS-CoV-2 Spike Protein Induces Cognitive Deficit and Anxiety-Like Behavior in Mouse via Non-cell Autonomous Hippocampal Neuronal Death,” Scientific Reports 2022, 12, 5496. doi: https://doi.org/10.1038/s41598-022-09410-7
173. Olajide OA et al., “Induction of Exaggerated Cytokine Production in Human Peripheral Blood Mononuclear Cells by a Recombinant SARS-CoV-2 Spike Glycoprotein S1 and Its Inhibition by Dexamethasone,” Inflammation 2021, 44: 1865–1877. doi: https://doi.org/10.1007/s10753-021-01464-5
174. Olajide OA et al., “SARS-CoV-2 spike glycoprotein S1 induces neuroinflammation in BV-2 microglia,” Mol. Neurobiol. 2022, 59: 445-458. doi: https://doi.org/10.1007/s12035-021-02593-6
175. Onnis A et al., “SARS-CoV-2 Spike protein suppresses CTL-mediated killing by inhibiting immune synapse assembly,” J Exp Med 2023, 220, 2: e20220906. doi: https://doi.org/10.1084/jem.20220906
176. Palestra F et al., “SARS-CoV-2 Spike Protein Activates Human Lung Macrophages,” Int. J. Mol. Sci. 2023, 24, 3: 3036. doi: https://doi.org/10.3390/ijms24033036
177. Pallas RM, “Innate and adaptative immune mechanisms of COVID-19 vaccines. Serious adverse events associated with SARS-CoV-2 vaccination: A systematic review,” Vacunas (English ed.) 2024, 25, 2: 285.e1-285.e94. doi: https://doi.org/10.1016/j.vacune.2024.05.002
178. Panigrahi S et al., “SARS-CoV-2 Spike Protein Destabilizes Microvascular Homeostasis,” Microbiol Spectr. 2021, 9, 3: e0073521. doi: https://doi.org/10.1128/Spectrum.00735-21
179. Park C et al., “Murine alveolar Macrophages Rapidly Accumulate intranasally Administered SARS-CoV-2 Spike Protein leading to neutrophil Recruitment and Damage,” Elife 2024, 12: RP86764. doi: https://doi.org/10.7554/eLife.86764.3
180. Park YJ et al., “D-dimer and CoV-2 spike-immune complexes contribute to the production of PGE2 and proinflammatory cytokines in monocytes,” PLoS Pathog. 2022, 18, 4: e1010468. doi: https://doi.org/10.1371/journal.ppat.1010468
181. Park YJ et al., “Pyrogenic and inflammatory mediators are produced by polarized M1 and M2 macrophages activated with D-dimer and SARS-CoV-2 spike immune complexes,” Cytokine 2024, 173: 156447. doi: https://doi.org/10.1016/j.cyto.2023.156447
182. Parry PL et al., “‘Spikeopathy’: COVID-19 Spike Protein Is Pathogenic, from Both Virus and Vaccine mRNA,” Biomedicine 2023, 11, 8: 2287. doi: https://doi.org/10.3390/biomedicines11082287
183. Passariello M et al., “Interactions of Spike-RBD of SARS-CoV-2 and Platelet Factor 4: New Insights in the Etiopathogenesis of Thrombosis,” Int. J. Mol. Sci. 2021, 22, 16: 8562. doi: https://doi.org/10.3390/ijms22168562
184. Patra T et al., “SARS-CoV-2 spike protein promotes IL-6 trans-signaling by activation of angiotensin II receptor signaling in epithelial cells,” PLoS Pathog. 2020, 16: e1009128. doi: https://doi.org/10.1371/journal.ppat.1009128
185. Patterson BK et al., “Persistence of SARS CoV-2 S1 Protein in CD16+ Monocytes in Post-Acute Sequelae of COVID-19 (PASC) up to 15 Months Post-Infection,” Front. Immunol. 12 (Sec. Viral Immunology). doi: https://doi.org/10.3389/fimmu.2021.746021
186. Pence B, “Recombinant SARS-CoV-2 Spike Protein Mediates Glycolytic and Inflammatory Activation in Human Monocytes,” Innov Aging 2020, 4, sp. 1: 955. doi: https://doi.org/10.1093/geroni/igaa057.3493
187. Perico L et al., “SARS-CoV-2 and the spike protein in endotheliopathy,” Trends Microbiol. 2024, 32, 1: 53-67. doi: 10.1016/j.tim.2023.06.004
188. Perico L et al., “SARS-CoV-2 Spike Protein 1 Activates Microvascular Endothelial Cells and Complement System Leading to Platelet Aggregation,” Front. Immunol. 2022, 13, 827146. doi: https://doi.org/10.3389/fimmu.2022.827146
189. Petrlova J et al., “SARS-CoV-2 spike protein aggregation is triggered by bacterial lipopolysaccharide,” FEBS Lett. 2022, 596: 2566–2575. doi: https://doi.org/10.1002/1873-3468.14490
190. Petrosino S and N Matende, “Elimination/Neutralization of COVID-19 Vaccine-Produced Spike Protein: Scoping Review,” Mathews Journal of Nutrition & Dietetics 2024, 7, 2. doi: https://doi.org/10.30654/MJND.10034
191. Petrovszki D et al., “Penetration of the SARS-CoV-2 Spike Protein across the Blood-Brain Barrier, as Revealed by a Combination of a Human Cell Culture Model System and Optical Biosensing,” Biomedicines 2022, 10, 1: 188. doi: https://doi.org/10.3390/biomedicines10010188
192. Petruk G et al., “SARS-CoV-2 spike protein binds to bacterial lipopolysaccharide and boosts proinflammatory activity,” J. Mol. Cell Biol. (2020) 12: 916-932. doi: https://doi.org/10.1093/jmcb/mjaa067
193. Prieto-Villalobos J et al., “SARS-CoV-2 spike protein S1 activates Cx43 hemichannels and disturbs intracellular Ca2+ dynamics,” Biol Res. 2023, 56, 1: 56. doi: https://doi.org/10.1186/s40659-023-00468-9
194. Puthia MTL et al., “Experimental model of pulmonary inflammation induced by SARS-CoV-2 spike protein and endotoxin,” ACS Pharmacol Transl Sci. 2022, 5, 3: 141–8. doi: https://doi.org/10.1021/acsptsci.1c00219
195. Raghavan S et al., “SARS-CoV-2 Spike Protein Induces Degradation of Junctional Proteins That Maintain Endothelial Barrier Integrity,” Front. Cardiovasc. Med. 2021, 8, 687783. doi: https://doi.org/10.3389/fcvm.2021.687783
196. Rahman M et al., “Differential Effect of SARS-CoV-2 Spike Glycoprotein 1 on Human Bronchial and Alveolar Lung Mucosa Models: Implications for Pathogenicity,” Viruses 2021, 13, 12: 2537. doi: https://doi.org/10.3390/v13122537
197. Rajah MM et al., “SARS-CoV-2 Alpha, Beta, and Delta variants display enhanced spike-mediated syncytia formation,” EMBO J. 2021, 40: e108944. doi: https://doi.org/10.15252/embj.2021108944
198. Ratajczak MZ et al., “SARS-CoV-2 Entry Receptor ACE2 Is Expressed on Very Small CD45– Precursors of Hematopoietic and Endothelial Cells and in Response to Virus Spike Protein Activates the Nlrp3 Inflammasome,” Stem Cell Rev Rep. 2021, 17, 1: 266-277. doi: https://doi.org/10.1007/s12015-020-10010-z
199. Robles JP et al., “The Spike Protein of SARS-CoV-2 Induces Endothelial Inflammation through Integrin α5β1 and NF-κB Signaling,” J. Biol. Chem. 2022, 298, 3: 101695. doi: https://doi.org/10.1016/j.jbc.2022.101695
200. Rong Z et al., “Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19,” Cell Host Microbe 2024, 26: S1931-3128(24)00438-4. doi: 10.1016/j.chom.2024.11.007
201. Ropa J et al., “Human Hematopoietic Stem, Progenitor, and Immune Cells Respond Ex Vivo to SARS-CoV-2 Spike Protein,” Stem Cell Rev Rep. 2021, 17, 1: 253-265. doi: https://doi.org/10.1007/s12015-020-10056-z
202. Rotoli BM et al., “Endothelial cell activation by SARS-CoV-2 spike S1 protein: A crosstalk between endothelium and innate immune cells,” Biomedicines 2021, 9, 9: 1220. doi: https://doi.org/10.3390/biomedicines9091220
203. Roytenberg R et al., “Thymidine phosphorylase mediates SARS-CoV-2 spike protein enhanced thrombosis in K18-hACE2TG mice,” Thromb. Res. 2024, 244, 8: 109195. doi: 10.1016/j.thromres.2024.109195
204. Ruben ML et al., “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am J Physiol Lung Cell Mol Physiol. 2021, 321, 2: L477-L484. doi: https://doi.org/10.1152/ajplung.00223.2021
205. Russo A, et al., “Implication of COVID-19 on Erythrocytes Functionality: Red Blood Cell Biochemical Implications and Morpho-Functional Aspects,” Int. J. Mol. Sci. 2022, 23, 4: 2171. doi: https://doi.org/10.3390/ijms23042171
206. Ryu JK et al., “Fibrin drives thromboinflammation and neuropathology in COVID-19,” Nature 2024, 633: 905-913. doi: https://doi.org/10.1038/s41586-024-07873-4
207. Saadi F et al., “Spike glycoprotein is central to coronavirus pathogenesis-parallel between m-CoV and SARS-CoV-2,” Ann Neurosci. 2021, 28 (3-4): 201–218. doi: https://doi.org/10.1177/09727531211023755
208. Samsudin S et al., “SARS-CoV-2 spike protein as a bacterial lipopolysaccharide delivery system in an overzealous inflammatory cascade,” J. Mol. Biol. 2022, 14, 9: mjac058. https://doi.org/10.1093/jmcb/mjac058
209. Sano H et al., “A case of persistent, confluent maculopapular erythema following a COVID-19 mRNA vaccination is possibly associated with the intralesional spike protein expressed by vascular endothelial cells and eccrine glands in the deep dermis,” J. Dermatol. 2023, 50: 1208–1212. doi: https://doi.org/10.1111/1346-8138.16816
210. Sano S et al., “SARS-CoV-2 spike protein found in the acrosyringium and eccrine gland of repetitive miliaria-like lesions in a woman following mRNA vaccination,” J. Dermatol. 2024, 51, 9: e293-e295. doi: https://doi.org/10.1111/1346-8138.17204
211. Santonja C et al., “COVID-19 chilblain-like lesion: immunohistochemical demonstration of SARS-CoV-2 spike protein in blood vessel endothelium and sweat gland epithelium in a polymerase chain reaction-negative patient,” Br J Dermatol. 2020, 183, 4: 778-780. doi: https://doi.org/10.1111/bjd.19338
212. Satta S et al., “An engineered nano-liposome-human ACE2 decoy neutralizes SARS-CoV-2 Spike protein-induced inflammation in both murine and human macrophages,” Theranostics 2022, 12, 6: 2639–2657. doi: 10.7150/thno.66831
213. Scheim DE, “A Deadly Embrace: Hemagglutination Mediated by SARS-CoV-2 Spike Protein at its 22 N-Glycosylation Sites, Red Blood Cell Surface Sialoglycoproteins, and Antibody,” Int. J. Mol. Sci. 2022, 23, 5, 2558. doi: https://doi.org/10.3390/ijms23052558
214. Scheim DE et al., “Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19,” Int. J. Mol. Schi. 2023, 24, 23:17039. doi: https://doi.org/10.3390/ijms242317039
215. Schroeder JT and AP Bieneman, “The S1 Subunit of the SARS-CoV-2 Spike protein activates human monocytes to produce cytokines linked to COVID-19: relevance to galectin-3,” Front Immunol. 2022, 13: 831763. doi: https://doi.org/10.3389/fimmu.2022.831763
216. Segura-Villalobos D et al., “Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein,” Pharmacol. Rep. 2022, 74: 1315–1325. doi: https://doi.org/10.1007/s43440-022-00398-5
217. Semmarath W et al., “Cyanidin-3-O-glucoside and Peonidin-3-O-glucoside-Rich Fraction of Black Rice Germ and Bran Suppresses Inflammatory Responses from SARS-CoV-2 Spike Glycoprotein S1-Induction In Vitro in A549 Lung Cells and THP-1 Macrophages via Inhibition of the NLRP3 Inflammasome Pathway,” Nutrients 2022, 14, 13: 2738. doi: https://doi.org/10.3390/nu14132738
218. Sharma VK et al., “Nanocurcumin Potently Inhibits SARS-CoV-2 Spike Protein-Induced Cytokine Storm by Deactivation of MAPK/NF-κB Signaling in Epithelial Cells,” ACS Appl. Bio Mater. 2022, 5, 2: 483–491. doi: https://doi.org/10.1021/acsabm.1c00874
219. Shirato K and Takako Kizaki, “SARS-CoV-2 Spike Protein S1 Subunit Induces Pro- inflammatory Responses via Toll-Like Receptor 4 Signaling in Murine and Human Macrophages,” Heliyon 2021, 7, 2: e06187. doi: https://doi.org/10.1016/j.heliyon.2021.e06187
220. Singh N and Anuradha Bharara Singh, “S2 Subunit of SARS-nCoV-2 Interacts with Tumor Suppressor Protein p53 and BRCA: An in Silico Study,” Transl. Oncol. 2020, 13, 10: 100814, doi: https://doi.org/10.1016/j.tranon.2020.100814
221. Singh RD, “The spike protein of sars-cov-2 induces heme oxygenase-1: pathophysiologic implications,” Biochim Biophys Acta, Mol Basis Dis 2022, 1868, 3: 166322. doi: https://doi.org/10.1016/j.bbadis.2021.166322
222. Sirsendu J et al., “Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells,” Int. J. Mol. Sci., 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
223. Soares CD et al., “Oral vesiculobullous lesions as an early sign of COVID‐19: immunohistochemical detection of SARS‐CoV‐2 spike protein,” Br. J. Dermatol. 2021, 184, 1: e6. doi: https://doi.org/10.1111/bjd.19569
224. Solis O et al., “The SARS-CoV-2 spike protein binds and modulates estrogen receptors,” Sci. Adv. 2022, 8, 48: eadd4150. doi: 10.1126/sciadv.add4150
225. Stern B et al., “SARS-CoV-2 spike protein induces endothelial dysfunction in 3D engineered vascular networks.” J. Biomed. Mater. Res. A. 2023, 112, 4: 524-533. doi: https://doi.org/10.1002/jbm.a.37543
226. Sui Y et al., “SARS-CoV-2 Spike Protein Suppresses ACE2 and Type I Interferon Expression in Primary Cells From Macaque Lung Bronchoalveolar Lavage,” Front. Immunol. 2021, 12. doi: https://doi.org/10.3389/fimmu.2021.658428
227. Sun Q et al., “SARS-coV-2 spike protein S1 exposure increases susceptibility to angiotensin II-induced hypertension in rats by promoting central neuroinflammation and oxidative stress,” Neurochem. Res. 2023, 48, 3016–3026. doi: https://doi.org/10.1007/s11064-023-03949-1
228. Sung PS et al., “CLEC5A and TLR2 Are Critical in SARS-CoV-2-Induced NET Formation and Lung Inflammation,” J. Biomed. Sci. 2002, 29, 52. doi: https://doi.org/10.1186/s12929-022-00832-z
229. Suprewicz L et al., “Blood-brain barrier function in response to SARS-CoV-2 and its spike protein,” Neurol. Neurochir Pol. 2023, 57: 14–25. doi: 10.5603/PJNNS.a2023.0014
230. Suprewicz L et al., “Recombinant human plasma gelsolin reverses increased permeability of the blood-brain barrier induced by the spike protein of the SARS-CoV-2 virus,” J Neuroinflammation 2022, 19, 1: 282, doi: https://doi.org/10.1186/s12974-022-02642-4
231. Suzuki YJ et al., “SARS-CoV-2 spike protein-mediated cell signaling in lung vascular cells,” Vascul. Pharmacol. 2021, 137: 106823. doi: https://doi.org/10.1016/j.vph.2020.106823
232. Suzuki YJ and SG Gychka, “SARS-CoV-2 Spike Protein Elicits Cell Signaling in Human Host Cells: Implications for Possible Consequences of COVID-19 Vaccines,” Vaccines 2021, 9, 1, 36. doi: https://doi.org/10.3390/vaccines9010036
233. Swank Z, et al. “Persistent Circulating Severe Acute Respiratory Syndrome Coronavirus 2 Spike Is Associated With Post-acute Coronavirus Disease 2019 Sequelae,” Clin. Infect. Dis. 2023, 76, 3: e487–e490. doi: https://doi.org/10.1093/cid/ciac722
234. Tetz G and Victor Tetz, “Prion-Like Domains in Spike Protein of SARS-CoV-2 Differ across Its Variants and Enable Changes in Affinity to ACE2,” Microorganisms 2022, 10, 2: 280, doi: https://doi.org/10.3390/microorganisms10020280
235. Theobald SJ et al., “Long-lived macrophage reprogramming drives spike protein-mediated inflammasome activation in COVID-19,” EMBO Mol. Med. 2021, 13: e14150. doi: https://doi.org/10.15252/emmm.202114150
236. Theoharides TC, “Could SARS-CoV-2 Spike Protein Be Responsible for Long-COVID Syndrome?” Mol. Neurobiol. 2022, 59, 3: 1850–1861. doi: https://doi.org/10.1007/s12035-021-02696-0
237. Theoharides TC and P Conti, “Be Aware of SARS-CoV-2 Spike Protein: There Is More Than Meets the Eye,” J. Biol. Reg. Homeost. Agents 2021, 35, 3: 833–838 doi: 10.23812/THEO_EDIT_3_21
238. Theuerkauf SA et al., “Quantitative assays reveal cell fusion at minimal levels of SARS-CoV-2 spike protein and fusion from without,” iScience 2021, 24, 3: 102170. doi: https://doi.org/10.1016/j.isci.2021.102170
239. Tillman TS et al., “SARS-CoV-2 Spike Protein Downregulates Cell Surface alpha7nAChR through a Helical Motif in the Spike Neck,” ACS Chem. Neurosci. 2023, 14, 4: 689–698. doi: https://doi.org/10.1021/acschemneuro.2c00610
240. Trougakos IP et al., “Adverse Effects of COVID-19 mRNA Vaccines: The Spike Hypothesis,” Trends Mol. Med. 2022, 28, 7: 542–554. doi: 10.1016/j.molmed.2022.04.007
241. Tyrkalska SD et al., “Differential proinflammatory activities of spike proteins of SARS-CoV-2 variants of concern,” Sci. Adv. 2022, 8, 37: eabo0732. doi: 10.1126/sciadv.abo0732
242. Vargas-Castro R et al., “Calcitriol prevents SARS-CoV spike-induced inflammation in human trophoblasts through downregulating ACE2 and TMPRSS2 expression,” J Steroid Biochem Mol Biol 2025, 245: 106625. doi: https://doi.org/10.1016/j.jsbmb.2024.106625
243. Vettori M et al., “Effects of Different Types of Recombinant SARS-CoV-2 Spike Protein on Circulating Monocytes’ Structure,” Int. J. Mol. Sci. 2023, 24, 11: 9373. doi: https://doi.org/10.3390/ijms24119373
244. Villacampa A et al., “SARS-CoV-2 S protein activates NLRP3 inflammasome and deregulates coagulation factors in endothelial and immune cells,” Cell Commun. Signal. 2024, 22, 38. doi: https://doi.org/10.1186/s12964-023-01397-6
245. Wang J et al., “SARS-CoV-2 Spike Protein S1 Domain Accelerates α-Synuclein Phosphorylation and Aggregation in Cellular Models of Synucleinopathy,” Mol Neurobiol. 2024, 61, 4:2446-2458. doi: https://doi.org/10.1007/s12035-023-03726-9
246. Wu ML et al., “Mast cell activation triggered by SARS-CoV-2 causes inflammation in brain microvascular endothelial cells and microglia,” Front. Cell. Infect. Microbiol., 2024, 14. doi: https://doi.org/10.3389/fcimb.2024.1358873
247. Yamamoto M et al., “Persistent varicella zoster virus infection following mRNA COVID-19 vaccination was associated with the presence of encoded spike protein in the lesion,” J. Cutan Immunol. Allergy. 2022:1–6. doi: https://doi.org/10.1002/cia2.12278
248. Yilmaz A et al., “Differential proinflammatory responses of colon epithelial cells to SARS-CoV-2 spike protein and Pseudomonas aeruginosa lipopolysaccharide,” Turk J Biochem. 2024. doi: https://doi.org/10.1515/tjb-2024-0144
249. Yonker LM et al., “Circulating Spike Protein Detected in Post–COVID-19 mRNA Vaccine Myocarditis,” Circulation 2023, 147, 11. doi: https://doi.org/10.1161/CIRCULATIONAHA.122.061025
250. Youn JY et al., “Therapeutic application of estrogen for COVID-19: Attenuation of SARS-CoV-2 spike protein and IL-6 stimulated, ACE2-dependent NOX2 activation, ROS production and MCP-1 upregulation in endothelial cells,” Redox Biol. 2021, 46: 102099. doi: https://doi.org/10.1016/j.redox.2021.102099
251. Youn YJ et al., “Nucleocapsid and spike proteins of SARS-CoV-2 drive neutrophil extracellular trap formation,” Immune Netw. 2021, 21, 2: e16. doi: https://doi.org/10.4110/in.2021.21.e16
252. Yu J et al., “Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition,” Blood 2020, 136, 18: 2080–2089. doi: https://doi.org/10.1182/blood.2020008248
253. Zaki H and S Khan, “SARS-CoV-2 spike protein induces inflammatory molecules through TLR2 in macrophages and monocytes,” J. Immunol. 2021, 206 (1_supplement): 62.07. doi: https://doi.org/10.4049/jimmunol.206.Supp.62.07
254. Zaki H and S Khan, “TLR2 senses spike protein of SARS-CoV-2 to trigger inflammation,”
J. Immunol. 2022, 208 (1_Supplement): 125.30. doi: https://doi.org/10.4049/jimmunol.208.Supp.125.30
255. Zekri-Nechar K et al., “Spike Protein Subunits of SARS-CoV-2 Alter Mitochondrial Metabolism in Human Pulmonary Microvascular Endothelial Cells: Involvement of Factor Xa,” Dis. Markers 2022: 1118195. doi: https://doi.org/10.1155/2022/1118195
256. Zeng FM et al., “SARS-CoV-2 spike spurs intestinal inflammation via VEGF production in enterocytes,” EMBO Mol Med. 2022, 14: e14844. doi: https://doi.org/10.15252/emmm.202114844
257. Zhang Q et al., “Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) membrane (M) and spike (S) proteins antagonize host type i interferon response,” Front Cell Infect Microbiol 2021, 11: 766922. doi: https://doi.org/10.3389/fcimb.2021.766922
258. Zhang RG et al., “SARS-CoV-2 spike protein receptor binding domain promotes IL-6 and IL-8 release via ATP/P2Y2 and ERK1/2 signaling pathways in human bronchial epithelia,” Mol. Immunol. 2024, 167: 53-61. doi: https://doi.org/10.1016/j.molimm.2024.02.005
259. Zhang S et al., “SARS-CoV-2 Binds Platelet ACE2 to Enhance Thrombosis in COVID-19,” J. Hematol. Oncol. 2020, 13, 120. doi: https://doi.org/10.1186/s13045-020-00954-7
260. Zhang Z et al., “SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination,” Cell Death Differ. 2021, 28: 2765–2777. doi: https://doi.org/10.1038/s41418-021-00782-3
261. Zhao Y et al., “SARS-CoV-2 spike protein interacts with and activates TLR4,” Cell Res. 2021, 31: 818–820. doi: https://doi.org/10.1038/s41422-021-00495-9
262. Zheng Y et al., “SARS-CoV-2 Spike Protein Causes Blood Coagulation and Thrombosis by Competitive Binding to Heparan Sulfate,” Int. J. Biol. Macromol. 2021, 193: 1124–1129, doi: https://doi.org/10.1016/j.ijbiomac.2021.10.112
263. Zhu G et al., “SARS-CoV-2 spike protein-induced host inflammatory response signature in human corneal epithelial cells,” Mol. Med. Rep. 2021, 24: 584. doi: https://doi.org/10.3892/mmr.2021.12223
II. CATEGORIES
A. General/Overview (20)
B. ACE2 (18)
C. Amyloid, prion-like properties (12)
D. Autoimmune (2)
E. Blood pressure/hypertension (2)
F. CD147 (13)
G. Cell membrane permeability, barrier dysfunction (13)
H. Cerebral, cerebrovascular, blood-brain barrier, cognitive (18)
I. Clinical pathology (19)
J. Clotting, platelets, hemoglobin (30)
K. Cytokines, chemokines, inteferon, interleukins (27)
L. Endothelial (25)
M. Gastrointestinal (6)
N. Immune dysfunction (4)
O. Macrophages, monocytes, neutrophils (28)
P. MAPK/NF-kB (10)
Q. Mast cells (3)
R. Microglia (6)
S. Microvascular (8)
T. Mitochondria/metabolism (8)
U. Myocarditis/cardiomyopathy (17)
V. NLRP3 (15)
W. Ocular, ophthalmic, conjunctival (3)
X. Other cell signaling (16)
Y. Pregnancy (3)
Z. Pulmonary, respiratory (26)
AA. Renin-Angiotensin-Aldosterone System (2)
BB. Senescence/aging (3)
CC. Stem cells (3)
DD. Syncytia/cell fusion (10)
EE. Therapeutics (35)
FF. Toll-like receptors (TLRs) (15)
A. General/Overview
1. Acevedo-Whitehouse K and R Bruno, “Potential health risks of mRNA-based vaccine therapy: A hypothesis,” Med. Hypotheses 2023, 171: 111015. doi: https://doi.org/10.1016/j.mehy.2023.111015
2. Almehdi AM et al., “SARS-CoV-2 Spike Protein: Pathogenesis, Vaccines, and Potential Therapies,” Infection 2021, 49, 5: 855–876. doi: https://doi.org/10.1007/s15010-021-01677-8
3. Baldari CT et al., “Emerging Roles of SARS-CoV-2 Spike-ACE2 in Immune Evasion and Pathogenesis,” Trends Immunol. 2023, 44, 6. doi: https://doi.org/10.1016/j.it.2023.04.001
4. Cosentino M and Franca Marino, “Understanding the Pharmacology of COVID- 19 mRNA Vaccines: Playing Dice with the Spike?” Int. J. Mol. Sci. 2022, 23, 18: 10881. doi: https://doi.org/10.3390/ijms231810881
5. Gussow AB et al., “Genomic Determinants of Pathogenicity in SARS-CoV-2 and Other Human Coronaviruses,” PNAS 117, 2020, 26: 15193–15199. doi: https://doi.org/10.1073/pnas.2008176117
6. Halma MTJ et al., “Strategies for the Management of Spike Protein-Related Pathology,” Microorganisms 2023, 11, 5: 1308, doi: https://doi.org/10.3390/microorganisms11051308
7. Kowarz E et al., “Vaccine-induced COVID-19 mimicry syndrome,” eLife 2022, 11: e74974. doi: https://doi.org/10.7554/eLife.74974
8. Lehmann KJ, “Impact of SARS-CoV-2 Spikes on Safety of Spike-Based COVID-19 Vaccinations,” Immunome Res. 2024, 20, 2: 1000267. doi: 10.35248/1745-7580.24.20.267
9. Lehmann KJ, “Suspected Causes of the Specific Intolerance Profile of Spike-Based Covid-19 Vaccines,” Med. Res. Arch 2024, 12, 9. doi: 10.18103/mra.v12i9.5704
10. Lesgard JF et al., “Toxicity of SARS-CoV-2 Spike Protein from the Virus and Produced from COVID-19 mRNA or Adenoviral DNA Vaccines,” Arch Microbiol Immun 2023, 7, 3: 121- 138. doi: 10.26502/ami.936500110
11. Letarov AV et al., “Free SARS-CoV-2 Spike Protein S1 Particles May Play a Role in the Pathogenesis of COVID-19 Infection,” Biochemistry (Moscow) 2021, 86, 257–261. doi: https://doi.org/10.1134/S0006297921030032
12. Nuovo JG et al., “Endothelial Cell Damage Is the Central Part of COVID-19 and a Mouse Model Induced by Injection of the S1 Subunit of the Spike Protein,” Ann. Diagn. Pathol. 2021, 51, 151682. doi: https://doi.org/10.1016/j.anndiagpath.2020.151682
13. Pallas RM, “Innate and adaptative immune mechanisms of COVID-19 vaccines. Serious adverse events associated with SARS-CoV-2 vaccination: A systematic review,” Vacunas (English ed.) 2024, 25, 2: 285.e1-285.e94. doi: https://doi.org/10.1016/j.vacune.2024.05.002
14. Parry PL et al., “‘Spikeopathy’: COVID-19 Spike Protein Is Pathogenic, from Both Virus and Vaccine mRNA,” Biomedicine 2023, 11, 8: 2287. doi: https://doi.org/10.3390/biomedicines11082287
15. Saadi F et al., “Spike glycoprotein is central to coronavirus pathogenesis-parallel between m-CoV and SARS-CoV-2,” Ann Neurosci. 2021, 28 (3-4): 201–218. doi: https://doi.org/10.1177/09727531211023755
16. Swank Z, et al. “Persistent Circulating Severe Acute Respiratory Syndrome Coronavirus 2 Spike Is Associated With Post-acute Coronavirus Disease 2019 Sequelae,” Clin. Infect. Dis 2023, 76, 3: e487–e490. doi: https://doi.org/10.1093/cid/ciac722
17. Theoharides TC, “Could SARS-CoV-2 Spike Protein Be Responsible for Long-COVID Syndrome?” Mol. Neurobiol. 2022, 59, 3: 1850–1861, doi: https://doi.org/10.1007/s12035-021-02696-0
18. Theoharides TC and P. Conti, “Be Aware of SARS-CoV-2 Spike Protein: There Is More Than Meets the Eye,” J Biol Reg Homeostat Agents 2021, 35, 3: 833–838 doi: 10.23812/THEO_EDIT_3_21
19. Trougakos IP et al., “Adverse Effects of COVID-19 mRNA Vaccines: The Spike Hypothesis,” Trends Mol Med. 2022, 28, 7: 542–554. doi: 10.1016/j.molmed.2022.04.007
20. Tyrkalska SD et al., “Differential proinflammatory activities of spike proteins of SARS-CoV-2 variants of concern,” Sci. Adv. 2022, 8, 37: eabo0732. doi: 10.1126/sciadv.abo0732
B. ACE2
1. Aboudounya MM and RJ Heads, “COVID-19 and Toll-Like Receptor 4 (TLR4): SARS-CoV-2 May Bind and Activate TLR4 to Increase ACE2 Expression, Facilitating Entry and Causing Hyperinflammation,” Mediators Inflamm. 2021, 8874339. doi: https://doi.org/10.1155/2021/8874339
2. Aksenova AY et al., “The increased amyloidogenicity of Spike RBD and pH-dependent binding to ACE2 may contribute to the transmissibility and pathogenic properties of SARS-CoV-2 omicron as suggested by in silico study,” Int J Mol Sci. 2022, 23, 21: 13502. doi: https://doi.org/10.3390/ijms232113502
3. Angeli F et al., “COVID-19, vaccines and deficiency of ACE2 and other angiotensinases. Closing the loop on the ‘Spike effect’,” Eur J. Intern. Med. 2022, 103: 23–28. doi: 10.1016/j.ejim.2022.06.015
4. Baldari CT et al., “Emerging Roles of SARS-CoV-2 Spike-ACE2 in Immune Evasion and Pathogenesis,” Trends Immunol. 2023, 44, 6. doi: https://doi.org/10.1016/j.it.2023.04.001
5. Devaux CA and L. Camoin-Jau, “Molecular mimicry of the viral spike in the SARS-CoV-2 vaccine possibly triggers transient dysregulation of ACE2, leading to vascular and coagulation dysfunction similar to SARS-CoV-2 infection,” Viruses 2023, 15, 5: 1045. doi: https://doi.org/10.3390/v15051045
6. Gao X et al., “Spike-Mediated ACE2 Down-Regulation Was Involved in the Pathogenesis of SARS-CoV-2 Infection,” J. Infect. 2022, 85, 4: 418–427. doi: 10.1016/j.jinf.2022.06.030
7. Kato Y et al., “TRPC3-Nox2 Protein Complex Formation Increases the Risk of SARS-CoV-2 Spike Protein-Induced Cardiomyocyte Dysfunction through ACE2 Upregulation,” Int. J. Mol. Sci. 2023, 24, 1: 102. doi: https://doi.org/10.3390/ijms24010102
8. Ken W et al., “Low dose radiation therapy attenuates ACE2 depression and inflammatory cytokines induction by COVID-19 viral spike protein in human bronchial epithelial cells,” Int J Radiat Biol. 2022, 98, 10: 1532-1541. doi: https://doi.org/10.1080/09553002.2022.2055806
9. Lei Y et al., “SARS-CoV-2 Spike Protein Impairs Endothelial Function via Downregulation of ACE 2,” Circulation Research 2021, 128, 9: 1323–1326. doi: https://doi.org/10.1161/CIRCRESAHA.121.318902
10. Lu J and PD Sun, “High affinity binding of SARS-CoV-2 spike protein enhances ACE2 carboxypeptidase activity,” J. Biol. Chem 2020, 295, 52: p18579-18588. doi: 10.1074/jbc.RA120.015303
11. Maeda Y et al., “Differential Ability of Spike Protein of SARS-CoV-2 Variants to Downregulate ACE2,” Int. J. Mol. Sci. 2024, 25, 2: 1353. doi: https://doi.org/10.3390/ijms25021353
12. Magro N et al., “Disruption of the blood-brain barrier is correlated with spike endocytosis by ACE2 + endothelia in the CNS microvasculature in fatal COVID-19. Scientific commentary on ‘Detection of blood-brain barrier disruption in brains of patients with COVID-19, but no evidence of brain penetration by SARS-CoV-2’,” Acta Neuropathol. 2024, 147, 1: 47. doi: https://doi.org/10.1007/s00401-023-02681-y
13. Satta S et al., “An engineered nano-liposome-human ACE2 decoy neutralizes SARS-CoV-2 Spike protein-induced inflammation in both murine and human macrophages,” Theranostics 2022, 12, 6: 2639–2657. doi: 10.7150/thno.66831
14. Sui Y et al., “SARS-CoV-2 Spike Protein Suppresses ACE2 and Type I Interferon Expression in Primary Cells From Macaque Lung Bronchoalveolar Lavage,” Front. Immunol. 2021, 12. doi: https://doi.org/10.3389/fimmu.2021.658428
15. Tetz G and Victor Tetz, “Prion-Like Domains in Spike Protein of SARS-CoV-2 Differ across Its Variants and Enable Changes in Affinity to ACE2,” Microorganisms 2025, 10, 2: 280. doi: https://doi.org/10.3390/microorganisms10020280
16. Vargas-Castro R et al., “Calcitriol prevents SARS-CoV spike-induced inflammation in human trophoblasts through downregulating ACE2 and TMPRSS2 expression,” J Steroid Biochem Mol Biol 2025, 245: 106625. doi: https://doi.org/10.1016/j.jsbmb.2024.106625
17. Youn JY et al., “Therapeutic application of estrogen for COVID-19: Attenuation of SARS-CoV-2 spike protein and IL-6 stimulated, ACE2-dependent NOX2 activation, ROS production and MCP-1 upregulation in endothelial cells,” Redox Biol. 2021, 46: 102099. doi: https://doi.org/10.1016/j.redox.2021.102099
18. Zhang S et al., “SARS-CoV-2 Binds Platelet ACE2 to Enhance Thrombosis in COVID-19,” J. Hematol. Oncol. 2020, 13, 120: 120. doi: https://doi.org/10.1186/s13045-020-00954-7
C. Amyloid, prion-like properties
1. Aksenova AY et al., “The increased amyloidogenicity of Spike RBD and pH-dependent binding to ACE2 may contribute to the transmissibility and pathogenic properties of SARS-CoV-2 omicron as suggested by in silico study,” Int. J. Mol. Sci. 2022, 23, 21: 13502. doi: https://doi.org/10.3390/ijms232113502
2. Cao S et al., “Spike Protein Fragments Promote Alzheimer’s Amyloidogenesis,” ACS Appl. Mater. Interfaces 2023, 15, 34: 40317-40329. doi: https://doi.org/10.1021/acsami.3c09815
3. Freeborn J, “Misfolded Spike Protein Could Explain Complicated COVID-19 Symptoms,” Medical News Today, May 26, 2022, https://www.medicalnewstoday.com/articles/misfolded-spike-protein-could-explain-complicated-covid-19-symptoms
4. Idrees D and Vijay Kumar, “SARS-CoV-2 Spike Protein Interactions with Amyloidogenic Proteins: Potential Clues to Neurodegeneration,” Biochemical and Biophysical Research Communications 2021, 554 : 94–98. doi: https://doi.org/10.1016/j.bbrc.2021.03.100
5. Ma G et al., “SARS-CoV-2 Spike protein S2 subunit modulates γ-secretase and enhances amyloid-β production in COVID-19 neuropathy,” Cell Discov 2022, 8, 99. doi: https://doi.org/10.1038/s41421-022-00458-3
6. Nahalka J, “1-L Transcription of SARS-CoV-2 Spike Protein S1 Subunit,” Int. J. Mol. Sci. 2024, 25, 8: 4440. doi: https://doi.org/10.3390/ijms25084440
7. Nyström S, “Amyloidogenesis of SARS-CoV-2 Spike Protein,” J. Am. Chem. Soc. 2022, 144, 8945–8950. doi: https://doi.org/10.1021/jacs.2c03925
8. Petrlova J et al., “SARS-CoV-2 spike protein aggregation is triggered by bacterial lipopolysaccharide,” FEBS Lett. 2022, 596:2566–2575. doi: https://doi.org/10.1002/1873-3468.14490
9. Petruk G et al., “SARS-CoV-2 spike protein binds to bacterial lipopolysaccharide and boosts proinflammatory activity,” J. Mol. Cell Biol. 2020, 12: 916-932. doi: https://doi.org/10.1093/jmcb/mjaa067
10. Rong Z et al., “Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19,” Cell Host Microbe 2024, 26: S1931-3128(24)00438-4. doi: 10.1016/j.chom.2024.11.007
11. Tetz G and Victor Tetz, “Prion-Like Domains in Spike Protein of SARS-CoV-2 Differ across Its Variants and Enable Changes in Affinity to ACE2,” Microorganisms 2022, 10, 2: 280, doi: https://doi.org/10.3390/microorganisms10020280
12. Wang J et al., “SARS-CoV-2 Spike Protein S1 Domain Accelerates α-Synuclein Phosphorylation and Aggregation in Cellular Models of Synucleinopathy,” Mol Neurobiol. 2024, 61, 4: 2446-2458. doi: https://doi.org/10.1007/s12035-023-03726-9
D. Autoimmune
1. Heil M, “Self-DNA driven inflammation in COVID-19 and after mRNA-based vaccination: lessons for non-COVID-19 pathologies,” Front. Immunol., 2023, 14. doi: https://doi.org/10.3389/fimmu.2023.1259879
2. Nunez-Castilla J et al., “Potential autoimmunity resulting from molecular mimicry between SARS-CoV-2 spike and human proteins,” Viruses 2022, 14, 7: 1415. https://doi.org/10.3390/v14071415
E. Blood pressure/hypertension
1. Angeli F et al., “The spike effect of acute respiratory syndrome coronavirus 2 and coronavirus disease 2019 vaccines on blood pressure,” Eur J Intern Med. 2023, 109: 12-21. doi: 10.1016/j.ejim.2022.12.004
2. Sun Q et al., “SARS-coV-2 spike protein S1 exposure increases susceptibility to angiotensin II-induced hypertension in rats by promoting central neuroinflammation and oxidative stress,” Neurochem. Res. 2023, 48, 3016–3026. doi: https://doi.org/10.1007/s11064-023-03949-1
F. CD147
1. Avolio E et al., “The SARS-CoV-2 Spike Protein Disrupts Human Cardiac Pericytes Function through CD147 Receptor-Mediated Signalling: A Potential Non-infective Mechanism of COVID-19 Microvascular Disease,” Clin. Sci. 2021, 135, 24: 2667–2689. doi: https://doi.org/10.1042/CS20210735
2. Loh D, “The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding,” Melatonin Research 2020, 3, 3: 380-416. doi: https://doi.org/10.32794/mr11250069
3. Maugeri N et al., “Unconventional CD147-Dependent Platelet Activation Elicited by SARS-CoV-2 in COVID-19,” J. Thromb. Haemost. 2021, 20, 2: 434–448. doi: https://doi.org/10.1111/jth.15575
G. Cell membrane permeability, barrier dysfunction
1. Asandei A et al., “Non-Receptor-Mediated Lipid Membrane Permeabilization by the SARS-CoV-2 Spike Protein S1 Subunit,” ACS Appl. Mater. Interfaces 2020, 12, 50: 55649–55658. doi: https://doi.org/10.1021/acsami.0c17044
2. Biancatelli RMLC, et al. “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Kappa18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am. J. Physiol. Lung Cell. Mol. Physiol. 2021, 321: L477–L484. doi: https://doi.org/10.1152/ajplung.00223.2021
3. Biering SB et al., “SARS-CoV-2 Spike Triggers Barrier Dysfunction and Vascular Leak via Integrins and TGF-β Signaling,” Nat. Commun. 2022, 13: 7630. doi: https://doi.org/10.1038/s41467-022-34910-5
4. Buzhdygan TP et al., “The SARS-CoV-2 Spike Protein Alters Barrier Function in 2D Static and 3D Microfluidic in-Vitro Models of the Human Blood-Brain Barrier,” Neurobiol. Dis. 2020, 146: 105131. doi: https://doi.org/10.1016/j.nbd.2020.105131
5. Chaves JCS et al., “Differential Cytokine Responses of APOE3 and APOE4 Blood–brain Barrier Cell Types to SARS-CoV-2 Spike Proteins,” J. Neuroimmune Pharmacol. 2024, 19, 22. doi: https://doi.org/10.1007/s11481-024-10127-9
6. Correa Y et al., “SARS-CoV-2 spike protein removes lipids from model membranes and interferes with the capacity of high-density lipoprotein to exchange lipids,” J. Colloid Interface Sci. 2021, 602: 732-739. doi: https://doi.org/10.1016/j.jcis.2021.06.056
7. DeOre BJ et al., “SARS-CoV-2 Spike Protein Disrupts Blood-Brain Barrier Integrity via RhoA Activation,” J Neuroimmune Pharmacol. 2021, 16, 4:722-728. Doi: https://doi.org/10.1007/s11481-021-10029-0
8. Guo Y and V Kanamarlapudi, “Molecular Analysis of SARS-CoV-2 Spike Protein-Induced Endothelial Cell Permeability and vWF Secretion,” Int. J. Mol. Sci. 2023, 24, 6: 5664. doi: https://doi.org/10.3390/ijms24065664
9. Luchini A et al., “Lipid bilayer degradation induced by SARS-CoV-2 spike protein as revealed by neutron reflectometry,” Sci. Rep. 2021, 11: 14867. doi: https://doi.org/10.1038/s41598-021-93996-x
10. Luo Y et al., “SARS-Cov-2 spike induces intestinal barrier dysfunction through the interaction between CEACAM5 and Galectin-9,” Front. Immunol. 2024, 15. doi: https://doi.org/10.3389/fimmu.2024.1303356
11. Magro N et al., “Disruption of the blood-brain barrier is correlated with spike endocytosis by ACE2 + endothelia in the CNS microvasculature in fatal COVID-19. Scientific commentary on ‘Detection of blood-brain barrier disruption in brains of patients with COVID-19, but no evidence of brain penetration by SARS-CoV-2’,” Acta Neuropathol. 2024, 147, 1: 47. doi: https://doi.org/10.1007/s00401-023-02681-y
12. Raghavan S et al., “SARS-CoV-2 Spike Protein Induces Degradation of Junctional Proteins That Maintain Endothelial Barrier Integrity,” Front. Cardiovasc. Med. 2021, 8, 687783. doi: https://doi.org/10.3389/fcvm.2021.687783
13. Ruben ML et al., “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am J Physiol Lung Cell Mol Physiol. 2021, 321, 2: L477-L484. doi: https://doi.org/10.1152/ajplung.00223.2021
H. Cerebral, cerebrovascular, blood-brain barrier, cognitive
1. Burnett FN et al., “SARS-CoV-2 Spike Protein Intensifies Cerebrovascular Complications in Diabetic hACE2 Mice through RAAS and TLR Signaling Activation,” Int. J. Mol. Sci. 2023, 24, 22: 16394. doi: https://doi.org/10.3390/ijms242216394
2. Choi JY et al., “SARS-CoV-2 spike S1 subunit protein-mediated increase of beta-secretase 1 (BACE1) impairs human brain vessel cells,” Biochem. Biophys. Res. Commun. 2022, 625, 20: 66-71. doi: https://doi.org/10.1016/j.bbrc.2022.07.113
3. Clough E et al., “Mitochondrial Dynamics in SARS-COV2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID,” J. Neuroimmune Pharmacol. 2021, 4, 16: 770–784. doi: https://doi.org/10.1007/s11481-021-10015-6
4. DeOre BJ et al., “SARS-CoV-2 Spike Protein Disrupts Blood-Brain Barrier Integrity via RhoA Activation,” J Neuroimmune Pharmacol. 2021, 16, 4: 722-728. Doi: https://doi.org/10.1007/s11481-021-10029-0
5. Erdogan MA, “Prenatal SARS-CoV-2 Spike Protein Exposure Induces Autism-Like Neurobehavioral Changes in Male Neonatal Rats,” J Neuroimmune Pharmacol. 2023, 18, 4: 573-591. doi: 10.1007/s11481-023-10089-4
6. Fontes-Dantas FL, “SARS-CoV-2 Spike Protein Induces TLR4-Mediated Long- Term Cognitive Dysfunction Recapitulating Post-COVID-19 Syndrome in Mice,” Cell Reports 2023, 42, 3: 112189. doi: https://doi.org/10.1016/j.celrep.2023.112189
7. Frank MG et al., “SARS-CoV-2 S1 subunit produces a protracted priming of the neuroinflammatory, physiological, and behavioral responses to a remote immune challenge: A role for corticosteroids,” Brain Behav. Immun. 2024, 121: 87-103. doi: https://doi.org/10.1016/j.bbi.2024.07.034
8. Heath SP et al., “SARS-CoV-2 Spike Protein Exacerbates Thromboembolic Cerebrovascular Complications in Humanized ACE2 Mouse Model,” Transl Stroke Res. 2024. doi: https://doi.org/10.1007/s12975-024-01301-5
9. Khaddaj-Mallat R et al., “SARS-CoV-2 deregulates the vascular and immune functions of brain pericytes via Spike protein,” Neurobiol. Dis. 2021, 161, 105561. doi: https://doi.org/10.1016/j.nbd.2021.105561
10. Kim ES et al., “Spike Proteins of SARS-CoV-2 Induce Pathological Changes in Molecular Delivery and Metabolic Function in the Brain Endothelial Cells,” Viruses 2021, 13, 10: 2021. doi: https://doi.org/10.3390/v13102021
11. Lykhmus O et al., “Immunization with 674–685 fragment of SARS-Cov-2 spike protein induces neuroinflammation and impairs episodic memory of mice,” Biochem. Biophys. Res. Commun. 2022, 622: 57–63. doi: https://doi.org/10.1016/j.bbrc.2022.07.016
12. Magro N et al., “Disruption of the blood-brain barrier is correlated with spike endocytosis by ACE2 + endothelia in the CNS microvasculature in fatal COVID-19. Scientific commentary on ‘Detection of blood-brain barrier disruption in brains of patients with COVID-19, but no evidence of brain penetration by SARS-CoV-2’,” Acta Neuropathol. 2024, 147, 1: 47. doi: https://doi.org/10.1007/s00401-023-02681-y
13. Oh J et al., “SARS-CoV-2 Spike Protein Induces Cognitive Deficit and Anxiety-Like Behavior in Mouse via Non-cell Autonomous Hippocampal Neuronal Death,” Scientific Reports 2022, 12, 5496. doi: https://doi.org/10.1038/s41598-022-09410-7
14. Petrovszki D et al., “Penetration of the SARS-CoV-2 Spike Protein across the Blood-Brain Barrier, as Revealed by a Combination of a Human Cell Culture Model System and Optical Biosensing,” Biomedicines 2022, 10, 1: 188. doi: https://doi.org/10.3390/biomedicines10010188
15. Rong Z et al., “Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19,” Cell Host Microbe 2024, 26: S1931-3128(24)00438-4. doi: 10.1016/j.chom.2024.11.007
16. Suprewicz L et al., “Blood-brain barrier function in response to SARS-CoV-2 and its spike protein,” Neurol. Neurochir Pol. 2023, 57: 14–25. doi: 10.5603/PJNNS.a2023.0014
17. Suprewicz L et al., “Recombinant human plasma gelsolin reverses increased permeability of the blood-brain barrier induced by the spike protein of the SARS-CoV-2 virus,” J Neuroinflammation 2022, 19, 1: 282, doi: https://doi.org/10.1186/s12974-022-02642-4
18. Wu ML et al., “Mast cell activation triggered by SARS-CoV-2 causes inflammation in brain microvascular endothelial cells and microglia,” Front. Cell. Infect. Microbiol., 2024, 14. doi: https://doi.org/10.3389/fcimb.2024.1358873
I. Clinical pathology
1. Baumeier C et al., “Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series,” Int. J. Mol. Sci. 2022, 23: 6940. doi: https://doi.org/10.3390/ijms23136940
2. Burkhardt A, “Pathology Conference: Vaccine-Induced Spike Protein Production in the Brain, Organs etc., now Proven,” Report24.news. 2022, https://report24.news/pathologie-konferenz-impfinduzierte-spike-produktion-in-gehirn-u-a-organen-nun-erwiesen/
3. Craddock V et al., “Persistent circulation of soluble and extracellular vesicle-linked Spike protein in individuals with postacute sequelae of COVID-19,” J Med. Virol. 2023, 95, 2: e28568. doi: https://doi.org/10.1002/jmv.28568
4. De Michele M et al., “Evidence of SARS-CoV-2 Spike Protein on Retrieved Thrombi from COVID-19 Patients,” J. Hematol. Oncol. 2022, 15, 108. doi: https://doi.org/10.1186/s13045-022-01329-w
5. De Sousa PMB et al., “Fatal Myocarditis following COVID-19 mRNA Immunization: A Case Report and Differential Diagnosis Review,” Vaccines 2024, 12, 2: 194. doi: https://doi.org/10.3390/vaccines12020194
6. Gamblicher T et al., “SARS‐CoV‐2 spike protein is present in both endothelial and eccrine cells of a chilblain‐like skin lesion,” J Eur Acad Dermatol Venereol. 2020, 1, 10: e187-e189. doi: https://doi.org/10.1111/jdv.16970
7. Gawaz A et al., “SARS-CoV-2–Induced Vasculitic Skin Lesions Are Associated with Massive Spike Protein Depositions in Autophagosomes,” J Invest Dermatol. 2024, 144, 2: 369-377.e4. doi: https://doi.org/10.1016/j.jid.2023.07.018
8. Hulscher N et al., “Autopsy findings in cases of fatal COVID-19 vaccine-induced myocarditis,” ESC Heart Failure 2024. doi: https://doi.org/10.1002/ehf2.14680
9. Ko CJ et al., “Discordant anti-SARS-CoV-2 spike protein and RNA staining in cutaneous perniotic lesions suggests endothelial deposition of cleaved spike protein,” J. Cutan Pathol 2021, 48, 1: 47–52. doi: https://doi.org/10.1111/cup.13866
10. Magen E et al., “Clinical and Molecular Characterization of a Rare Case of BNT162b2 mRNA COVID-19 Vaccine-Associated Myositis,” Vaccines 2022, 10: 1135. doi: https://doi.org/10.3390/vaccines10071135
11. Magro N et al., “Disruption of the blood-brain barrier is correlated with spike endocytosis by ACE2 + endothelia in the CNS microvasculature in fatal COVID-19. Scientific commentary on ‘Detection of blood-brain barrier disruption in brains of patients with COVID-19, but no evidence of brain penetration by SARS-CoV-2’,” Acta Neuropathol. 2024, 147, 1: 47. doi: https://doi.org/10.1007/s00401-023-02681-y
12. Mörz M, “A Case Report: Multifocal Necrotizing Encephalitis and Myocarditis after BNT162b2 mRNA Vaccination against COVID-19,” Vaccines 2022, 10, 10: 1651. doi: https://doi.org/10.3390/vaccines10101651
13. Rong Z et al., “Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19,” Cell Host Microbe 2024, 26: S1931-3128(24)00438-4. doi: 10.1016/j.chom.2024.11.007
14. Sano H et al., “A case of persistent, confluent maculopapular erythema following a COVID-19 mRNA vaccination is possibly associated with the intralesional spike protein expressed by vascular endothelial cells and eccrine glands in the deep dermis,” J. Dermatol. 2023, 50: 1208–1212. doi: https://doi.org/10.1111/1346-8138.16816
15. Sano S et al., “SARS-CoV-2 spike protein found in the acrosyringium and eccrine gland of repetitive miliaria-like lesions in a woman following mRNA vaccination,” J. Dermatol. 2024, 51, 9: e293-e295. doi: https://doi.org/10.1111/1346-8138.17204
16. Santonja C et al., “COVID-19 chilblain-like lesion: immunohistochemical demonstration of SARS-CoV-2 spike protein in blood vessel endothelium and sweat gland epithelium in a polymerase chain reaction-negative patient,” Br J Dermatol. 2020, 183, 4: 778-780. doi: https://doi.org/10.1111/bjd.19338
17. Soares CD et al., “Oral vesiculobullous lesions as an early sign of COVID‐19: immunohistochemical detection of SARS‐CoV‐2 spike protein,” Br. J. Dermatol. 2021, 184, 1: e6. doi: https://doi.org/10.1111/bjd.19569
18. Yamamoto M et al., “Persistent varicella zoster virus infection following mRNA COVID-19 vaccination was associated with the presence of encoded spike protein in the lesion,” J. Cutan Immunol. Allergy. 2022: 1-6. doi: https://doi.org/10.1002/cia2.12278
19. Yonker LM et al., “Circulating Spike Protein Detected in Post–COVID-19 mRNA Vaccine Myocarditis,” Circulation 2023, 147, 11. doi: https://doi.org/10.1161/CIRCULATIONAHA.122.061025
J. Clotting, platelets, hemoglobin
1. Al-Kuraishy HM et al., “Changes in the Blood Viscosity in Patients With SARS-CoV-2 Infection,” Front. Med. 2022, 9: 876017. doi: 10.3389/fmed.2022.876017
2. Al-Kuraishy HM et al., “Hemolytic anemia in COVID-19,” Ann. Hematol. 2022, 101: 1887–1895. doi: 10.1007/s00277-022-04907-7
3. Appelbaum K et al., “SARS-CoV-2 spike-dependent platelet activation in COVID-19 vaccine-induced thrombocytopenia,” Blood Adv. 2022, 6: 2250–2253. doi: 10.1182/bloodadvances.2021005050
4. Boschi C et al., “SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects,” Int. J. Biol. Macromol. 2022, 23, 24: 15480, doi: https://doi.org/10.3390/ijms232415480
5. Bye AP et al., “Aberrant glycosylation of anti-SARS-CoV-2 spike IgG is a prothrombotic stimulus for platelets,” Blood 2021, 138, 6: 1481–9. doi: https://doi.org/10.1182/blood.2021011871
6. Carnevale R et al., “Toll-Like Receptor 4-Dependent Platelet-Related Thrombosis in SARS-CoV-2 Infection,” Circ. Res. 2023, 132, 3: 290– 305, doi: https://doi.org/10.1161/CIRCRESAHA.122.321541
7. Cossenza LC et al., “Inhibitory effects of SARS-CoV-2 spike protein and BNT162b2 vaccine on erythropoietin-induced globin gene expression in erythroid precursor cells from patients with β-thalassemia,” Exp. Hematol. 2024, 129, 104128. doi: https://doi.org/10.1016/j.exphem.2023.11.002
8. De Michele M et al., “Vaccine-induced immune thrombotic thrombocytopenia: a possible pathogenic role of ChAdOx1 nCoV-19 vaccine-encoded soluble SARS-CoV-2 spike protein,” Haematologica 2022, 107, 7: 1687–92. https://doi.org/10.3324/haematol.2021.280180
9. Grobbelaar LM et al., “SARS-CoV-2 Spike Protein S1 Induces Fibrin(ogen) Resistant to Fibrinolysis: Implications for Microclot Formation in COVID-19,” Biosicence Reports 2021, 41, 8: BSR20210611. doi: https://doi.org/10.1042/BSR20210611
10. Heath SP et al., “SARS-CoV-2 Spike Protein Exacerbates Thromboembolic Cerebrovascular Complications in Humanized ACE2 Mouse Model,” Transl Stroke Res. 2024. doi: https://doi.org/10.1007/s12975-024-01301-5
11. Iba T and JH Levy, “The roles of platelets in COVID-19-associated coagulopathy and vaccine-induced immune thrombotic thrombocytopenia,” Trends Cardiovasc Med. 2022, 32, 1: 1-9. doi: https://doi.org/10.1016/j.tcm.2021.08.012
12. Huynh TV et al., “Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling,” Cells 2024, 13, 16: 1331. doi: https://doi.org/10.3390/cells13161331
13. Iba T and JH Levy, “The roles of platelets in COVID-19-associated coagulopathy and vaccine-induced immune thrombotic thrombocytopenia,” Trends Cardiovasc Med. 2022, 32, 1: 1-9. doi: https://doi.org/10.1016/j.tcm.2021.08.012
14. Jana S et al., “Cell-free hemoglobin does not attenuate the effects of SARS-CoV-2 spike protein S1 subunit in pulmonary endothelial cells,” Int. J. Mol. Sci. 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
15. Kim SY et al., “Characterization of heparin and severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) spike glycoprotein binding interactions,” Antivir Res. 2020, 181: 104873. doi: https://doi.org/10.1016/j.antiviral.2020.104873
16. Kircheis R, “Coagulopathies after Vaccination against SARS-CoV-2 May Be Derived from a Combined Effect of SARS-CoV-2 Spike Protein and Adenovirus Vector-Triggered Signaling Pathways,” Int. J. Mol. Sci. 2021, 22, 19: 10791. https://doi.org/10.3390/ijms221910791
17. Kuhn CC et al. “Direct Cryo-ET observation of platelet deformation induced by SARS-CoV-2 spike protein,” Nat. Commun. 2023, 14, 620. doi: https://doi.org/10.1038/s41467-023-36279-5
18. Li T et al., “Platelets Mediate Inflammatory Monocyte Activation by SARS-CoV-2 Spike Protein,” J. Clin. Invest. 2022, 132, 4: e150101. doi: 10.1172/JCI150101
19. Maugeri N et al., “Unconventional CD147-Dependent Platelet Activation Elicited by SARS-CoV-2 in COVID-19,” J. Thromb. Haemost. 2021, 20, 2: 434–448, doi: https://doi.org/10.1111/jth.15575
20. Passariello M et al., “Interactions of Spike-RBD of SARS-CoV-2 and Platelet Factor 4: New Insights in the Etiopathogenesis of Thrombosis,” Int. J. Mol. Sci. 2021, 22, 16: 8562. doi: https://doi.org/10.3390/ijms22168562
21. Perico L et al., “SARS-CoV-2 Spike Protein 1 Activates Microvascular Endothelial Cells and Complement System Leading to Platelet Aggregation,” Front. Immunol. 2022, 13, 827146. doi: https://doi.org/10.3389/fimmu.2022.827146
22. Roytenberg R et al., “Thymidine phosphorylase mediates SARS-CoV-2 spike protein enhanced thrombosis in K18-hACE2TG mice,” Thromb. Res. 2024, 244, 8: 109195. doi: 10.1016/j.thromres.2024.109195
23. Russo A, et al., “Implication of COVID-19 on Erythrocytes Functionality: Red Blood Cell Biochemical Implications and Morpho-Functional Aspects,” Int. J. Mol. Sci. 2022, 23, 4: 2171. doi: https://doi.org/10.3390/ijms23042171
24. Ryu JK et al., “Fibrin drives thromboinflammation and neuropathology in COVID-19,” Nature 2024, 633: 905-913. doi: https://doi.org/10.1038/s41586-024-07873-4
25. Scheim, DE. “A Deadly Embrace: Hemagglutination Mediated by SARS-CoV-2 Spike Protein at its 22 N-Glycosylation Sites, Red Blood Cell Surface Sialoglycoproteins, and Antibody,” Int. J. Mol. Sci. 2022, 23, 5: 2558. doi: https://doi.org/10.3390/ijms23052558
26. Scheim DE et al., “Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19,” Int. J. Mol. Sci. 2023, 24, 23: 17039. doi: https://doi.org/10.3390/ijms242317039
27. Sirsendu J et al., “Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells,” Int. J. Mol. Sci., 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
28. Zhang S et al., “SARS-CoV-2 Binds Platelet ACE2 to Enhance Thrombosis in COVID-19,” J. Hematol. Oncol. 2020, 13, 120: 120. doi: https://doi.org/10.1186/s13045-020-00954-7
29. Zhang Z et al., “SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination,” Cell Death Differ. 2021, 28, 2765–2777. doi: https://doi.org/10.1038/s41418-021-00782-3
30. Zheng Y et al., “SARS-CoV-2 Spike Protein Causes Blood Coagulation and Thrombosis by Competitive Binding to Heparan Sulfate,” Int. J. Biol. Macromol. 2021, 193: 1124–1129. doi: https://doi.org/10.1016/j.ijbiomac.2021.10.112
K. Cytokines, chemokines, inteferon, interleukins
1. Ao Z et al., “SARS-CoV-2 Delta spike protein enhances the viral fusogenicity and inflammatory cytokine production,” iScience 2022, 25, 8: 104759. doi: 10.1016/j.isci.2022.104759
2. Chaves JCS et al., “Differential Cytokine Responses of APOE3 and APOE4 Blood–brain Barrier Cell Types to SARS-CoV-2 Spike Proteins,” J. Neuroimmune Pharmacol. 2024, 19, 22. doi: https://doi.org/10.1007/s11481-024-10127-9
3. Chittasupho C et al., “Targeting spike glycoprotein S1 mediated by NLRP3 inflammasome machinery and the cytokine releases in A549 lung epithelial cells by nanocurcumin,” Pharmaceuticals (Basel) 2023, 16, 6: 862. doi: https://doi.org/10.3390/ph16060862
4. Das T et al., “N-glycosylation of the SARS-CoV-2 spike protein at Asn331 and Asn343 is involved in spike-ACE2 binding, virus entry, and regulation of IL-6,” Microbiol. Immunol. 2024, 68, 5: 165-178. doi: https://doi.org/10.1111/1348-0421.13121
5. Duarte C, “Age-dependent effects of the recombinant spike protein/SARS-CoV-2 on the M-CSF- and IL-34-differentiated macrophages in vitro,” Biochem. Biophys. Res. Commun. 2021, 546: 97–102. doi: https://doi.org/10.1016/j.bbrc.2021.01.104
6. Forsyth CB et al., “The SARS-CoV-2 S1 spike protein promotes MAPK and NF-kB activation in human lung cells and inflammatory cytokine production in human lung and intestinal epithelial cells,” Microorganisms 2022, 10, 10: 1996. doi: https://doi.org/10.3390/microorganisms10101996
7. Freitas RS et al., “SARS-CoV-2 Spike antagonizes innate antiviral immunity by targeting interferon regulatory factor 3,” Front Cell Infect Microbiol. 2021, 11: 789462. doi: https://doi.org/10.3389/fcimb.2021.789462
8. Gasparello J et al., “Sulforaphane inhibits the expression of interleukin-6 and interleukin-8 induced in bronchial epithelial IB3-1 cells by exposure to the SARS-CoV-2 Spike protein,” Phytomedicine 2021, 87: 153583. doi: https://doi.org/10.1016/j.phymed.2021.153583
9. Ghazanfari D et al., “Mechanistic insights into SARS-CoV-2 spike protein induction of the chemokine CXCL10,” Sci. Rep. 2024, 14: 11179. doi: https://doi.org/10.1038/s41598-024-61906-6
10. Gracie NP et al., “Cellular signalling by SARS-CoV-2 spike protein,” Microbiology Australia 2024, 45, 1: 13-17. doi: https://doi.org/10.1071/MA24005
11. Gu T et al., “Cytokine Signature Induced by SARS-CoV-2 Spike Protein in a Mouse Model,” Front. Immunol., 2021 (Sec. Inflammation). doi: https://doi.org/10.3389/fimmu.2020.621441
12. Jugler C et al, “SARS-CoV-2 Spike Protein-Induced Interleukin 6 Signaling Is Blocked by a Plant-Produced Anti-Interleukin 6 Receptor Monoclonal Antibody,” Vaccines 2021, 9, 11: 1365. https://doi.org/10.3390/vaccines9111365
13. Liang S et al., “SARS-CoV-2 spike protein induces IL-18-mediated cardiopulmonary inflammation via reduced mitophagy,” Signal Transduct Target Ther 2023, 8, 103. doi: https://doi.org/10.1038/s41392-023-01368-w
14. Liu T et al., “RS-5645 attenuates inflammatory cytokine storm induced by SARS-CoV-2 spike protein and LPS by modulating pulmonary microbiota,” Int. J. Biol. Sci. 2021, 17, 13: 3305–3319. doi: 10.7150/ijbs.63329
15. Liu X et al., “SARS-CoV-2 spike protein-induced cell fusion activates the cGAS-STING pathway and the interferon response,” Sci Signal. 2022, 15, 729: eabg8744. doi: 10.1126/scisignal.abg8744
16. Niu C et al., “SARS-CoV-2 spike protein induces the cytokine release syndrome by stimulating T cells to produce more IL-2,” Front. Immunol. 2024, 15: 1444643. doi: https://doi.org/10.3389/fimmu.2024.1444643
17. Norris B et al., “Evaluation of Glutathione in Spike Protein of SARS-CoV-2 Induced Immunothrombosis and Cytokine Dysregulation,” Antioxidants 2024, 13, 3: 271. doi: https://doi.org/10.3390/antiox13030271
18. Olajide OA et al., “Induction of Exaggerated Cytokine Production in Human Peripheral Blood Mononuclear Cells by a Recombinant SARS-CoV-2 Spike Glycoprotein S1 and Its Inhibition by Dexamethasone,” Inflammation 2021, 44: 1865–1877. doi: https://doi.org/10.1007/s10753-021-01464-5
19. Park YJ et al., “D-dimer and CoV-2 spike-immune complexes contribute to the production of PGE2 and proinflammatory cytokines in monocytes,” PLoS Pathog., 2022, 18, 4: e1010468. doi: https://doi.org/10.1371/journal.ppat.1010468
20. Patra T et al., “SARS-CoV-2 spike protein promotes IL-6 trans-signaling by activation of angiotensin II receptor signaling in epithelial cells,” PLoS Pathog. 2020, 16: e1009128. doi: https://doi.org/10.1371/journal.ppat.1009128
21. Samsudin S et al., “SARS-CoV-2 spike protein as a bacterial lipopolysaccharide delivery system in an overzealous inflammatory cascade,” J. Mol. Biol. 2022, 14, 9: mjac058. doi: https://doi.org/10.1093/jmcb/mjac058
22. Schroeder JT and AP Bieneman, “The S1 Subunit of the SARS-CoV-2 Spike protein activates human monocytes to produce cytokines linked to COVID-19: relevance to galectin-3,” Front Immunol. 2022, 13: 831763. doi: https://doi.org/10.3389/fimmu.2022.831763
23. Sharma VK et al., “Nanocurcumin Potently Inhibits SARS-CoV-2 Spike Protein-Induced Cytokine Storm by Deactivation of MAPK/NF-κB Signaling in Epithelial Cells,” ACS Appl. Bio Mater. 2022, 5, 2: 483–491. doi: https://doi.org/10.1021/acsabm.1c00874
24. Sui Y et al., “SARS-CoV-2 Spike Protein Suppresses ACE2 and Type I Interferon Expression in Primary Cells From Macaque Lung Bronchoalveolar Lavage,” Front. Immunol. 2021, 12. doi: https://doi.org/10.3389/fimmu.2021.658428
25. Youn JY et al., “Therapeutic application of estrogen for COVID-19: Attenuation of SARS-CoV-2 spike protein and IL-6 stimulated, ACE2-dependent NOX2 activation, ROS production and MCP-1 upregulation in endothelial cells,” Redox Biol. 2021, 46: 102099. doi: https://doi.org/10.1016/j.redox.2021.102099
26. Zhang Q et al., “Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) membrane (M) and spike (S) proteins antagonize host type i interferon response,” Front Cell Infect Microbiol 2021, 11: 766922. doi: https://doi.org/10.3389/fcimb.2021.766922
27. Zhang RG et al., “SARS-CoV-2 spike protein receptor binding domain promotes IL-6 and IL-8 release via ATP/P2Y2 and ERK1/2 signaling pathways in human bronchial epithelia,” Mol. Immunol. 2024, 167: 53-61. doi: https://doi.org/10.1016/j.molimm.2024.02.005
L. Endothelial
1. Bhargavan B and GD Kanmogne, “SARS-CoV-2 spike proteins and cell–cell communication inhibits TFPI and induces thrombogenic factors in human lung microvascular endothelial cells and neutrophils: implications for COVID-19 coagulopathy pathogenesis,” Int. J. Mol. Sci. 2022, 23, 18: 10436. doi: https://doi.org/10.3390/ijms231810436
2. Biancatelli RMLC, et al. “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Kappa18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am. J. Physiol. Lung Cell. Mol. Physiol. 2021, 321: L477–L484. doi: https://doi.org/10.1152/ajplung.00223.2021
3. Gamblicher T et al., “SARS‐CoV‐2 spike protein is present in both endothelial and eccrine cells of a chilblain‐like skin lesion,” J Eur Acad Dermatol Venereol. 2020, 1, 10: e187-e189. doi: https://doi.org/10.1111/jdv.16970
4. Guo Y and V Kanamarlapudi, “Molecular Analysis of SARS-CoV-2 Spike Protein-Induced Endothelial Cell Permeability and vWF Secretion,” Int. J. Mol. Sci. 2023, 24, 6: 5664. doi: https://doi.org/10.3390/ijms24065664
5. Jana S et al., “Cell-free hemoglobin does not attenuate the effects of SARS-CoV-2 spike protein S1 subunit in pulmonary endothelial cells,” Int. J. Mol. Sci. 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
6. Kulkoviene G et al., “Differential Mitochondrial, Oxidative Stress and Inflammatory Responses to SARS-CoV-2 Spike Protein Receptor Binding Domain in Human Lung Microvascular, Coronary Artery Endothelial and Bronchial Epithelial Cells,” Int. J. Mol. Sci. 2024, 25, 6: 3188. doi: https://doi.org/10.3390/ijms25063188
7. Marrone L et al., “Tirofiban prevents the effects of SARS-CoV-2 spike protein on macrophage activation and endothelial cell death,” Heliyon, 2024, 10, 15, e35341. doi: 10.1016/j.heliyon.2024.e35341
8. Meyer K et al., “SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells,” J. Virol. 2021, 95: e0079421. doi: https://doi.org/10.1128/jvi.00794-21
9. Nuovo JG et al., “Endothelial Cell Damage Is the Central Part of COVID-19 and a Mouse Model Induced by Injection of the S1 Subunit of the Spike Protein,” Ann. Diagn. Pathol. 2021, 51, 151682. doi: https://doi.org/10.1016/j.anndiagpath.2020.151682
10. Perico L et al., “SARS-CoV-2 and the spike protein in endotheliopathy,” Trends Microbiol. 2024, 32, 1: 53-67. doi: 10.1016/j.tim.2023.06.004
11. Perico L et al., “SARS-CoV-2 Spike Protein 1 Activates Microvascular Endothelial Cells and Complement System Leading to Platelet Aggregation,” Front. Immunol. 2022, 13, 827146. doi: https://doi.org/10.3389/fimmu.2022.827146
12. Raghavan S et al., “SARS-CoV-2 Spike Protein Induces Degradation of Junctional Proteins That Maintain Endothelial Barrier Integrity,” Front. Cardiovasc. Med. 2021, 8, 687783. doi: https://doi.org/10.3389/fcvm.2021.687783
13. Ratajczak MZ et al., “SARS-CoV-2 Entry Receptor ACE2 Is Expressed on Very Small CD45– Precursors of Hematopoietic and Endothelial Cells and in Response to Virus Spike Protein Activates the Nlrp3 Inflammasome,” Stem Cell Rev Rep. 2021, 17, 1: 266-277. doi: https://doi.org/10.1007/s12015-020-10010-z
14. Robles JP et al., “The Spike Protein of SARS-CoV-2 Induces Endothelial Inflammation through Integrin α5β1 and NF-κB Signaling,” J. Biol. Chem. 2022, 298, 3: 101695. doi: https://doi.org/10.1016/j.jbc.2022.101695
15. Rotoli BM et al., “Endothelial cell activation by SARS-CoV-2 spike S1 protein: A crosstalk between endothelium and innate immune cells,” Biomedicines 2021, 9, 9: 1220. doi: https://doi.org/10.3390/biomedicines9091220
16. Ruben ML et al., “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am J Physiol Lung Cell Mol Physiol. 2021, 321, 2: L477-L484. doi: https://doi.org/10.1152/ajplung.00223.2021
17. Sano H et al., “A case of persistent, confluent maculopapular erythema following a COVID-19 mRNA vaccination is possibly associated with the intralesional spike protein expressed by vascular endothelial cells and eccrine glands in the deep dermis,” J. Dermatol. 2023, 50: 1208–1212. doi: https://doi.org/10.1111/1346-8138.16816
18. Santonja C et al., “COVID-19 chilblain-like lesion: immunohistochemical demonstration of SARS-CoV-2 spike protein in blood vessel endothelium and sweat gland epithelium in a polymerase chain reaction-negative patient,” Br J Dermatol. 2020, 183, 4: 778-780. doi: https://doi.org/10.1111/bjd.19338
19. Scheim DE et al., “Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19,” Int. J. Mol. Sci. 2023, 24, 23: 17039. doi: https://doi.org/10.3390/ijms242317039
20. Sirsendu J et al., “Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells,” Int. J. Mol. Sci., 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
21. Stern B et al., “SARS-CoV-2 spike protein induces endothelial dysfunction in 3D engineered vascular networks,” J. Biomed. Mater. Res. A. 2023, 112, 4: 524-533. doi: https://doi.org/10.1002/jbm.a.37543
22. Villacampa A et al., “SARS-CoV-2 S protein activates NLRP3 inflammasome and deregulates coagulation factors in endothelial and immune cells,” Cell Commun. Signal. 2024, 22, 38. doi: https://doi.org/10.1186/s12964-023-01397-6
23. Wu ML et al., “Mast cell activation triggered by SARS-CoV-2 causes inflammation in brain microvascular endothelial cells and microglia,” Front. Cell. Infect. Microbiol. 2024, 14. doi: https://doi.org/10.3389/fcimb.2024.1358873
24. Youn JY et al., “Therapeutic application of estrogen for COVID-19: Attenuation of SARS-CoV-2 spike protein and IL-6 stimulated, ACE2-dependent NOX2 activation, ROS production and MCP-1 upregulation in endothelial cells,” Redox Biol. 2021, 46: 102099. doi: https://doi.org/10.1016/j.redox.2021.102099
25. Zekri-Nechar K et al., “Spike Protein Subunits of SARS-CoV-2 Alter Mitochondrial Metabolism in Human Pulmonary Microvascular Endothelial Cells: Involvement of Factor Xa,” Dis. Markers 2022, 1118195. doi: https://doi.org/10.1155/2022/1118195
M. Gastrointestinal
1. Forsyth CB et al., “The SARS-CoV-2 S1 spike protein promotes MAPK and NF-kB activation in human lung cells and inflammatory cytokine production in human lung and intestinal epithelial cells,” Microorganisms 2022, 10, 10: 1996. doi: https://doi.org/10.3390/microorganisms10101996
2. Li Z et al., “SARS-CoV-2 pathogenesis in the gastrointestinal tract mediated by Spike-induced intestinal inflammation,” Precis. Clin. Med. 2024, 7, 1: pbad034. doi: https://doi.org/10.1093/pcmedi/pbad034
3. Luo Y et al., “SARS-Cov-2 spike induces intestinal barrier dysfunction through the interaction between CEACAM5 and Galectin-9,” Front. Immunol. 2024, 15. doi: https://doi.org/10.3389/fimmu.2024.1303356
4. Nascimento RR et al., “SARS-CoV-2 Spike protein triggers gut impairment since mucosal barrier to innermost layers: From basic science to clinical relevance,” Mucosal Immunol. 2024, 17, 4: 565-583. doi: https://doi.org/10.1016/j.mucimm.2024.03.00
5. Yilmaz A et al., “Differential proinflammatory responses of colon epithelial cells to SARS-CoV-2 spike protein and Pseudomonas aeruginosa lipopolysaccharide,” Turk J Biochem. 2024. doi: https://doi.org/10.1515/tjb-2024-0144
6. Zeng FM et al., “SARS-CoV-2 spike spurs intestinal inflammation via VEGF production in enterocytes,” EMBO Mol Med. 2022, 14: e14844. doi: https://doi.org/10.15252/emmm.202114844
N. Immune dysfunction
1. Baldari CT et al., “Emerging Roles of SARS-CoV-2 Spike-ACE2 in Immune Evasion and Pathogenesis,” Trends Immunol. 2023, 44, 6. doi: https://doi.org/10.1016/j.it.2023.04.001
2. Bocquet-Garcon A, “Impact of the SARS-CoV-2 Spike Protein on the Innate Immune System: A Review,” Cureus 2024, 16, 3: e57008. doi: 10.7759/cureus.57008
3. Kim MJ et al., “The SARS‐CoV‐2 spike protein induces lung cancer migration and invasion in a TLR2‐dependent manner,” Cancer Commun (London), 2023, 44, 2: 273–277. doi: https://doi.org/10.1002/cac2.12485
4. Onnis A et al., “SARS-CoV-2 Spike protein suppresses CTL-mediated killing by inhibiting immune synapse assembly,” J Exp Med 2023, 220, 2: e20220906. doi: https://doi.org/10.1084/jem.20220906
O. Macrophages, monocytes, neutrophils
1. Ahn WM et al., “SARS-CoV-2 Spike Protein Stimulates Macropinocytosis in Murine and Human Macrophages via PKC-NADPH Oxidase Signaling,” Antioxidants 2024, 13, 2: 175. doi: https://doi.org/10.3390/antiox13020175
2. Ait-Belkacem I et al., “SARS-CoV-2 spike protein induces a differential monocyte activation that may contribute to age bias in COVID-19 severity,” Sci. Rep. 2022, 12: 20824. doi: https://doi.org/10.1038/s41598-022-25259-2
3. Barhoumi T et al., “SARS-CoV-2 coronavirus Spike protein-induced apoptosis, inflammatory, and oxidative stress responses in THP-1-like-macrophages: potential role of angiotensin-converting enzyme inhibitor (perindopril),” Front. Immunol. 2021, 12: 728896. doi: https://doi.org/10.3389/fimmu.2021.728896
4. Bortolotti D et al., “SARS-CoV-2 Spike 1 Protein Controls Natural Killer Cell Activation via the HLA-E/NKG2A Pathway,” Cells 2020, 9, 9: 1975. doi: https://doi.org/10.3390/cells9091975
5. Cao X et al., “Spike protein of SARS-CoV-2 activates macrophages and contributes to induction of acute lung inflammation in male mice,” FASEB J. 2021, 35, e21801. doi: https://doi.org/10.1096/fj.202002742RR
6. Chiok K et al., “Proinflammatory Responses in SARS-CoV-2 and Soluble Spike Glycoprotein S1 Subunit Activated Human Macrophages,” Viruses 2023, 15, 3: 754. doi: https://doi.org/10.3390/v15030754
7. Cory TJ et al., “Metformin Suppresses Monocyte Immunometabolic Activation by SARS-CoV-2 Spike Protein Subunit 1,” Front. Immunol. 2021, 12 (Sec. Cytokines and Soluble Mediators in Immunity): 733921. doi: https://doi.org/10.3389/fimmu.2021.733921
8. Del Re A et al., “Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages,” Metabolites 2021, 11, 9: 592. doi: https://doi.org/10.3390/metabo11090592
9. Duarte C, “Age-dependent effects of the recombinant spike protein/SARS-CoV-2 on the M-CSF- and IL-34-differentiated macrophages in vitro,” Biochem. Biophys. Res. Commun. 2021, 546: 97–102. doi: https://doi.org/10.1016/j.bbrc.2021.01.104
10. Karwaciak I et al., “Nucleocapsid and Spike Proteins of the Coronavirus Sars-Cov-2 Induce Il6 in Monocytes and Macrophages—Potential Implications for Cytokine Storm Syndrome,” Vaccines 2021, 9, 1, 54: 1–10. doi: https://doi.org/10.3390/vaccines9010054
11. Li T et al., “Platelets Mediate Inflammatory Monocyte Activation by SARS-CoV-2 Spike Protein,” J. Clin. Invest. 2022, 132, 4: e150101. doi: 10.1172/JCI150101
12. Loh JT et al., “Dok3 restrains neutrophil production of calprotectin during TLR4 sensing of SARS-CoV-2 spike protein,” Front. Immunol. 2022, 13 (Sec. Molecular Innate Immunity). doi: https://doi.org/10.3389/fimmu.2022.996637
13. Marrone L et al., “Tirofiban prevents the effects of SARS-CoV-2 spike protein on macrophage activation and endothelial cell death,” Heliyon, 2024, 10, 15: e35341. doi: 10.1016/j.heliyon.2024.e35341
14. Miller GM et al., “SARS-CoV-2 and SARS-CoV-2 Spike protein S1 subunit Trigger Proinflammatory Response in Macrophages in the Absence of Productive Infection,” J. Immunol. 2023, 210 (1_Supplement): 71.30. doi: https://doi.org/10.4049/jimmunol.210.Supp.71.30
15. Onnis A et al., “SARS-CoV-2 Spike protein suppresses CTL-mediated killing by inhibiting immune synapse assembly,” J Exp Med 2023, 220, 2: e20220906. doi: https://doi.org/10.1084/jem.20220906
16. Palestra F et al. “SARS-CoV-2 Spike Protein Activates Human Lung Macrophages,” Int. J. Mol. Sci. 2023, 24, 3: 3036. doi: https://doi.org/10.3390/ijms24033036
17. Park C et al., “Murine alveolar Macrophages Rapidly Accumulate intranasally Administered SARS-CoV-2 Spike Protein leading to neutrophil Recruitment and Damage,” Elife 2024, 12, RP86764. doi: https://doi.org/10.7554/eLife.86764.3
18. Park YJ et al., “D-dimer and CoV-2 spike-immune complexes contribute to the production of PGE2 and proinflammatory cytokines in monocytes,” PLoS Pathog. 2022, 18, 4: e1010468. doi: https://doi.org/10.1371/journal.ppat.1010468
19. Park YJ et al., “Pyrogenic and inflammatory mediators are produced by polarized M1 and M2 macrophages activated with D-dimer and SARS-CoV-2 spike immune complexes,” Cytokine 2024, 173: 156447. doi: https://doi.org/10.1016/j.cyto.2023.156447
20. Patterson BK et al., “Persistence of SARS CoV-2 S1 Protein in CD16+ Monocytes in Post-Acute Sequelae of COVID-19 (PASC) up to 15 Months Post-Infection,” Front. Immunol. 12 (Sec. Viral Immunology). doi: https://doi.org/10.3389/fimmu.2021.746021
21. Pence B, “Recombinant SARS-CoV-2 Spike Protein Mediates Glycolytic and Inflammatory Activation in Human Monocytes,” Innov Aging 2020, 4, sp. 1: 955. doi: https://doi.org/10.1093/geroni/igaa057.3493
22. Satta S et al., “An engineered nano-liposome-human ACE2 decoy neutralizes SARS-CoV-2 Spike protein-induced inflammation in both murine and human macrophages,” Theranostics 2022, 12, 6: 2639–2657. doi: 10.7150/thno.66831
23. Schroeder JT and AP Bieneman, “The S1 Subunit of the SARS-CoV-2 Spike protein activates human monocytes to produce cytokines linked to COVID-19: relevance to galectin-3,” Front Immunol. 2022, 13: 831763. doi: https://doi.org/10.3389/fimmu.2022.831763
24. Shirato K and Takako Kizaki, “SARS-CoV-2 Spike Protein S1 Subunit Induces Pro- inflammatory Responses via Toll-Like Receptor 4 Signaling in Murine and Human Macrophages,” Heliyon 2021, 7, 2: e06187, doi: https://doi.org/10.1016/j.heliyon.2021.e06187
25. Theobald SJ et al., “Long-lived macrophage reprogramming drives spike protein-mediated inflammasome activation in COVID-19,” EMBO Mol. Med. 2021, 13:e14150. doi: https://doi.org/10.15252/emmm.202114150
26. Vettori M et al., “Effects of Different Types of Recombinant SARS-CoV-2 Spike Protein on Circulating Monocytes’ Structure,” Int. J. Mol. Sci. 2023, 24, 11, 9373. doi: https://doi.org/10.3390/ijms24119373
27. Youn YJ et al., “Nucleocapsid and spike proteins of SARS-CoV-2 drive neutrophil extracellular trap formation,” Immune Netw. 2021, 21, 2: e16. doi: https://doi.org/10.4110/in.2021.21.e16
28. Zaki H and S Khan, “SARS-CoV-2 spike protein induces inflammatory molecules through TLR2 in macrophages and monocytes,” J. Immunol. 2021, 206 (1_supplement): 62.07. doi: https://doi.org/10.4049/jimmunol.206.Supp.62.07
P. MAPK/NF-kB
1. Arjsri P et al., “Hesperetin from root extract of Clerodendrum petasites S. Moore inhibits SARS-CoV-2 spike protein S1 subunit-induced Nlrp3 inflammasome in A549 lung cells via modulation of the Akt/Mapk/Ap-1 pathway,” Int. J. Mol. Sci. 2022, 23, 18: 10346. doi: https://doi.org/10.3390/ijms231810346
2. Bhattacharyya S and JK Tobacman, “SARS-CoV-2 spike protein-ACE2 interaction increases carbohydrate sulfotransferases and reduces N-acetylgalactosamine-4-sulfatase by p38 MAPK,” Signal Transduct Target Ther 2024, 9, 39. doi: https://doi.org/10.1038/s41392-024-01741-3
3. Forsyth CB et al., “The SARS-CoV-2 S1 spike protein promotes MAPK and NF-kB activation in human lung cells and inflammatory cytokine production in human lung and intestinal epithelial cells,” Microorganisms 2022, 10, 10: 1996. doi: https://doi.org/10.3390/microorganisms10101996
4. Johnson EL et al., “The S1 spike protein of SARS-CoV-2 upregulates the ERK/MAPK signaling pathway in DC-SIGN-expressing THP-1 cells,” Cell Stress Chaperones 2024, 29, 2: 227-234. doi: https://doi.org/10.1016/j.cstres.2024.03.002
5. Khan S et al., “SARS-CoV-2 Spike Protein Induces Inflammation via TLR2-Dependent Activation of the NF-κB Pathway,” eLife 2021, 10: e68563, doi: https://doi.org/10.7554/elife.68563
6. Kircheis R and O Planz, “Could a Lower Toll-like Receptor (TLR) and NF-κB Activation Due to a Changed Charge Distribution in the Spike Protein Be the Reason for the Lower Pathogenicity of Omicron?” Int. J. Mol. Sci. 2022, 23, 11: 5966. doi: https://doi.org/10.3390/ijms23115966
7. Kyriakopoulos AM et al., “Mitogen Activated Protein Kinase (MAPK) Activation, p53, and Autophagy Inhibition Characterize the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Protein Induced Neurotoxicity,” Cureus 2022, 14, 12: e32361. doi: 10.7759/cureus.32361
8. Robles JP et al., “The Spike Protein of SARS-CoV-2 Induces Endothelial Inflammation through Integrin α5β1 and NF-κB Signaling,” J. Biol. Chem. 2022, 298, 3: 101695. doi: https://doi.org/10.1016/j.jbc.2022.101695
9. Sharma VK et al., “Nanocurcumin Potently Inhibits SARS-CoV-2 Spike Protein-Induced Cytokine Storm by Deactivation of MAPK/NF-κB Signaling in Epithelial Cells,” ACS Appl. Bio Mater. 2022, 5, 2: 483–491. doi: https://doi.org/10.1021/acsabm.1c00874
10. Bhattacharyya S and JK Tobacman, “SARS-CoV-2 spike protein-ACE2 interaction increases carbohydrate sulfotransferases and reduces N-acetylgalactosamine-4-sulfatase by p38 MAPK,” Signal Transduct Target Ther 2024, 9, 39. doi: https://doi.org/10.1038/s41392-024-01741-3
Q. Mast cells
1. Cao JB et al., “Mast cell degranulation-triggered by SARS-CoV-2 induces tracheal-bronchial epithelial inflammation and injury,” Virol. Sin. 2024, 39, 2: 309-318. doi: https://doi.org/10.1016/j.virs.2024.03.001
2. Fajloun Z et al., “SARS-CoV-2 or Vaccinal Spike Protein can Induce Mast Cell Activation Syndrome (MCAS),” Infect Disord Drug Targets, 2025, 25, 1: e300424229561. doi: 10.2174/0118715265319896240427045026
3. Wu ML et al., “Mast cell activation triggered by SARS-CoV-2 causes inflammation in brain microvascular endothelial cells and microglia,” Front. Cell. Infect. Microbiol., 2024, 14. doi: https://doi.org/10.3389/fcimb.2024.1358873
R. Microglia
1. Chang MH et al., “SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin,” Biomedicines 2024, 12, 6: 1223. doi: https://doi.org/10.3390/biomedicines12061223
2. Clough E et al., “Mitochondrial Dynamics in SARS-COV2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID,” J. Neuroimmune Pharmacol. 2021, 16, 4: 770–784. doi: https://doi.org/10.1007/s11481-021-10015-6
3. Frank MG et al., “SARS-CoV-2 Spike S1 Subunit Induces Neuroinflammatory, Microglial and Behavioral Sickness Responses: Evidence of PAMP-Like Properties,” Brain Behav. Immun. 2022, 100: 267277. doi: https://doi.org/10.1016/j.bbi.2021.12.007
4. Mishra R and AC Banerjea, “SARS-CoV-2 Spike targets USP33-IRF9 axis via exosomal miR-148a to activate human microglia,” Front. Immunol. 2021, 12: 656700. doi: https://doi.org/10.3389/fimmu.2021.656700
5. Olajide OA et al., “SARS-CoV-2 spike glycoprotein S1 induces neuroinflammation in BV-2 microglia,”
Mol. Neurobiol. 2022, 59: 445-458. doi: https://doi.org/10.1007/s12035-021-02593-6
6. Wu ML et al., “Mast cell activation triggered by SARS-CoV-2 causes inflammation in brain microvascular endothelial cells and microglia,” Front. Cell. Infect. Microbiol. 2024, 14. doi: https://doi.org/10.3389/fcimb.2024.1358873
S. Microvascular
1. Avolio E et al., “The SARS-CoV-2 Spike Protein Disrupts Human Cardiac Pericytes Function through CD147 Receptor-Mediated Signalling: A Potential Non-infective Mechanism of COVID-19 Microvascular Disease,” Clin. Sci. 2021, 135, 24: 2667–2689. doi: https://doi.org/10.1042/CS20210735
2. Bhargavan B and GD Kanmogne, “SARS-CoV-2 spike proteins and cell–cell communication inhibits TFPI and induces thrombogenic factors in human lung microvascular endothelial cells and neutrophils: implications for COVID-19 coagulopathy pathogenesis,” Int. J. Mol. Sci. 2022, 23, 18: 10436. doi: https://doi.org/10.3390/ijms231810436
3. Kulkoviene G et al., “Differential Mitochondrial, Oxidative Stress and Inflammatory Responses to SARS-CoV-2 Spike Protein Receptor Binding Domain in Human Lung Microvascular, Coronary Artery Endothelial and Bronchial Epithelial Cells,” Int. J. Mol. Sci. 2024, 25, 6: 3188. doi: https://doi.org/10.3390/ijms25063188
4. Magro N et al., “Disruption of the blood-brain barrier is correlated with spike endocytosis by ACE2 + endothelia in the CNS microvasculature in fatal COVID-19. Scientific commentary on ‘Detection of blood-brain barrier disruption in brains of patients with COVID-19, but no evidence of brain penetration by SARS-CoV-2’,” Acta Neuropathol. 2024, 147, 1: 47. doi: https://doi.org/10.1007/s00401-023-02681-y
5. Panigrahi S et al., “SARS-CoV-2 Spike Protein Destabilizes Microvascular Homeostasis,” Microbiol Spectr. 2021, 9, 3: e0073521. doi: https://doi.org/10.1128/Spectrum.00735-21
6. Perico L et al., “SARS-CoV-2 Spike Protein 1 Activates Microvascular Endothelial Cells and Complement System Leading to Platelet Aggregation,” Front. Immunol. 2022, 13, 827146. doi: https://doi.org/10.3389/fimmu.2022.827146
7. Wu ML et al., “Mast cell activation triggered by SARS-CoV-2 causes inflammation in brain microvascular endothelial cells and microglia,” Front. Cell. Infect. Microbiol. 2024, 14. doi: https://doi.org/10.3389/fcimb.2024.1358873
8. Zekri-Nechar K et al., “Spike Protein Subunits of SARS-CoV-2 Alter Mitochondrial Metabolism in Human Pulmonary Microvascular Endothelial Cells: Involvement of Factor Xa,” Dis. Markers 2022: 1118195. doi: https://doi.org/10.1155/2022/1118195
T. Mitochondria/metabolism
1. Cao X et al., “The SARS-CoV-2 spike protein induces long-term transcriptional perturbations of mitochondrial metabolic genes, causes cardiac fibrosis, and reduces myocardial contractile in obese mice,” Mol. Metab. 2023, 74, 101756. doi: https://doi.org/10.1016/j.molmet.2023.101756
2. Chang MH et al., “SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin,” Biomedicines 2024, 12, 6: 1223. doi: https://doi.org/10.3390/biomedicines12061223
3. Clough E et al., “Mitochondrial Dynamics in SARS-COV2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID,” Journal of Neuroimmune Pharmacology 2021, 16, 4: 770–784. doi: https://doi.org/10.1007/s11481-021-10015-6
4. Huynh TV et al., “Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19,” Cells 2023, 12, 877. doi: https://doi.org/10.3390/cells12060877
5. Kulkoviene G et al., “Differential Mitochondrial, Oxidative Stress and Inflammatory Responses to SARS-CoV-2 Spike Protein Receptor Binding Domain in Human Lung Microvascular, Coronary Artery Endothelial and Bronchial Epithelial Cells,” Int. J. Mol. Sci. 2024, 25, 6: 3188. doi: https://doi.org/10.3390/ijms25063188
6. Mercado-Gómez M et al., “The spike of SARS-CoV-2 promotes metabolic rewiring in hepatocytes,” Commun. Biol. 2022, 5, 827. doi: https://doi.org/10.1038/s42003-022-03789-9
7. Nguyen V, “The Spike Protein of SARS-CoV-2 Impairs Lipid Metabolism and Increases Susceptibility to Lipotoxicity: Implication for a Role of Nrf2,” Cells 2022, 11, 12: 1916. doi: https://doi.org/10.3390/cells11121916
8. Zekri-Nechar K et al., “Spike Protein Subunits of SARS-CoV-2 Alter Mitochondrial Metabolism in Human Pulmonary Microvascular Endothelial Cells: Involvement of Factor Xa,” Dis. Markers 2022, 1118195. doi: https://doi.org/10.1155/2022/1118195
U. Myocarditis/cardiomyopathy
1. Avolio E et al., “The SARS-CoV-2 Spike Protein Disrupts Human Cardiac Pericytes Function through CD147 Receptor-Mediated Signalling: A Potential Non-infective Mechanism of COVID-19 Microvascular Disease,” Clin. Sci. 2021, 135, 24: 2667–2689. doi: https://doi.org/10.1042/CS20210735
2. Baumeier C et al., “Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series,” Int. J. Mol. Sci. 2022, 23: 6940. doi: https://doi.org/10.3390/ijms23136940
3. Bellavite P et al., “Immune response and molecular mechanisms of cardiovascular adverse effects of spike proteins from SARS-coV-2 and mRNA vaccines,” Biomedicines 2023, 11, 2: 451. doi: https://doi.org/10.3390/biomedicines11020451
4. Boretti A. “PQQ Supplementation and SARS-CoV-2 Spike Protein-Induced Heart Inflammation,” Nat. Prod. Commun. 2022, 17, 1934578×221080929. doi: https://doi.org/10.1177/1934578X221080929
5. Buoninfante A et al., “Myocarditis associated with COVID-19 vaccination,” npj Vaccines 2024, 122. doi: https://doi.org/10.1038/s41541-024-00893-1
6. Cao X et al., “The SARS-CoV-2 spike protein induces long-term transcriptional perturbations of mitochondrial metabolic genes, causes cardiac fibrosis, and reduces myocardial contractile in obese mice,” Mol. Metab. 2023, 74, 101756. doi: https://doi.org/10.1016/j.molmet.2023.101756
7. Clemens DJ et al., “SARS-CoV-2 spike protein-mediated cardiomyocyte fusion may contribute to increased arrhythmic risk in COVID-19,” PLoS One 2023, 18, 3: e0282151. doi: https://doi.org/10.1371/journal.pone.0282151
8. De Sousa PMB et al., “Fatal Myocarditis following COVID-19 mRNA Immunization: A Case Report and Differential Diagnosis Review,” Vaccines 2024, 12, 2: 194. doi: https://doi.org/10.3390/vaccines12020194
9. Forte E, “Circulating spike protein may contribute to myocarditis after COVID-19 vaccination,” Nat. Cardiovasc. Res. 2023, 2: 100. doi: https://doi.org/10.1038/s44161-023-00222-0
10. Huang X et al., “Sars-Cov-2 Spike Protein-Induced Damage of hiPSC-Derived Cardiomyocytes,” Adv. Biol. 2022, 6, 7: e2101327. doi: https://doi.org/10.1002/adbi.202101327
11. Hulscher N et al., “Autopsy findings in cases of fatal COVID-19 vaccine-induced myocarditis,” ESC Heart Failure 2024. doi: https://doi.org/10.1002/ehf2.14680
12. Huynh TV et al., “Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19,” Cells 2023, 12, 877. doi: https://doi.org/10.3390/cells12060877
13. Huynh TV et al., “Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling,” Cells 2024, 13, 16: 1331. doi: https://doi.org/10.3390/cells13161331
14. Imig JD, “SARS-CoV-2 spike protein causes cardiovascular disease independent of viral infection,” Clin Sci (Lond) 2022, 136, 6: 431–434. doi: https://doi.org/10.1042/CS20220028
15. Kato Y et al., “TRPC3-Nox2 Protein Complex Formation Increases the Risk of SARS-CoV-2 Spike Protein-Induced Cardiomyocyte Dysfunction through ACE2 Upregulation,” Int. J. Mol. Sci. 2023, 24, 1: 102. doi: https://doi.org/10.3390/ijms24010102
16. Lin Z, “More than a key—the pathological roles of SARS-CoV-2 spike protein in COVID-19 related cardiac injury,” Sports Med Health Sci 2023, 6, 3: 209-220. doi: https://doi.org/10.1016/j.smhs.2023.03.004
17. Yonker LM et al., “Circulating Spike Protein Detected in Post–COVID-19 mRNA Vaccine Myocarditis,” Circulation 2023, 147, 11. doi: https://doi.org/10.1161/CIRCULATIONAHA.122.061025
V. NLRP3
1. Albornoz EA et al., “SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein,” Mol. Psychiatr. 2023, 28: 2878–2893. doi: https://doi.org/10.1038/s41380-022-01831-0
2. Arjsri P et al., “Hesperetin from root extract of Clerodendrum petasites S. Moore inhibits SARS-CoV-2 spike protein S1 subunit-induced Nlrp3 inflammasome in A549 lung cells via modulation of the Akt/Mapk/Ap-1 pathway,” Int. J. Mol. Sci. 2022, 23, 18: 10346. doi: https://doi.org/10.3390/ijms231810346
3. Chittasupho C et al., “Inhibition of SARS-CoV-2-Induced NLRP3 Inflammasome-Mediated Lung Cell Inflammation by Triphala-Loaded Nanoparticle Targeting Spike Glycoprotein S1,” Pharmaceutics 2024, 16, 6: 751. https://doi.org/10.3390/pharmaceutics16060751
4. Chittasupho C et al., “Targeting spike glycoprotein S1 mediated by NLRP3 inflammasome machinery and the cytokine releases in A549 lung epithelial cells by nanocurcumin,” Pharmaceuticals (Basel) 2023, 16, 6: 862. doi: https://doi.org/10.3390/ph16060862
7. Corpetti C et al., “Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line,” Phytother. Res. 2021, 35, 12: 6893–6903. doi: https://doi.org/10.1002/ptr.7302
8. Del Re A et al., “Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages.” Metabolites 2021, 11, 9: 592. dsoi: https://doi.org/10.3390/metabo11090592
9. Dissook S et al., “Luteolin-rich fraction from Perilla frutescens seed meal inhibits spike glycoprotein S1 of SARS-CoV-2-induced NLRP3 inflammasome lung cell inflammation via regulation of JAK1/STAT3 pathway: A potential anti-inflammatory compound against inflammation-induced long-COVID,” Front. Med. 2023, 9: 1072056. doi: https://doi.org/10.3389/fmed.2022.1072056
10. Huynh TV et al., “Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling,” Cells 2024, 13, 16: 1331. doi: https://doi.org/10.3390/cells13161331
11. Jiang Q et al., “SARS-CoV-2 spike S1 protein induces microglial NLRP3-dependent neuroinflammation and cognitive impairment in mice,” Exp. Neurol. 2025, 383: 115020. doi: https://doi.org/10.1016/j.expneurol.2024.115020
12. Kucia M et al. “An evidence that SARS-Cov-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner,” Leukemia 2021, 35: 3026-3029. doi: https://doi.org/10.1038/s41375-021-01332-z
13. Ratajczak MZ et al., “SARS-CoV-2 Entry Receptor ACE2 Is Expressed on Very Small CD45– Precursors of Hematopoietic and Endothelial Cells and in Response to Virus Spike Protein Activates the Nlrp3 Inflammasome,” Stem Cell Rev Rep. 2021, 17, 1: 266-277. doi: https://doi.org/10.1007/s12015-020-10010-z
14. Semmarath W et al., “Cyanidin-3-O-glucoside and Peonidin-3-O-glucoside-Rich Fraction of Black Rice Germ and Bran Suppresses Inflammatory Responses from SARS-CoV-2 Spike Glycoprotein S1-Induction In Vitro in A549 Lung Cells and THP-1 Macrophages via Inhibition of the NLRP3 Inflammasome Pathway,” Nutrients 2022, 14, 13: 2738. doi: https://doi.org/10.3390/nu14132738
15. Villacampa A et al., “SARS-CoV-2 S protein activates NLRP3 inflammasome and deregulates coagulation factors in endothelial and immune cells,” Cell Commun. Signal. 2024, 22, 38. doi: https://doi.org/10.1186/s12964-023-01397-6
W. Ocular, ophthalmic, conjunctival
1. Golob-Schwarzl N et al., “SARS-CoV-2 spike protein functionally interacts with primary human conjunctival epithelial cells to induce a pro-inflammatory response,” Eye 2022, 36: 2353–5. doi: https://doi.org/10.1038/s41433-022-02066-7
2. Grishma K and Das Sarma, “The Role of Coronavirus Spike Protein in Inducing Optic Neuritis in Mice: Parallels to the SARS-CoV-2 Virus,” J Neuroophthalmol 2024, 44, 3: 319-329. doi: 10.1097/WNO.0000000000002234
3. Zhu G et al., “SARS-CoV-2 spike protein-induced host inflammatory response signature in human corneal epithelial cells,” Mol. Med. Rep. 2021, 24: 584. doi: https://doi.org/10.3892/mmr.2021.12223
X. Other cell signaling
1. Caohuy H et al., “Inflammation in the COVID-19 airway is due to inhibition of CFTR signaling by the SARS-CoV-2 spike protein,” Sci. Rep. 2024, 14: 16895. doi: https://doi.org/10.1038/s41598-024-66473-4
2. Choi JY et al., “SARS-CoV-2 spike S1 subunit protein-mediated increase of beta-secretase 1 (BACE1) impairs human brain vessel cells,” Biochem. Biophys. Res. Commun. 2022, 625, 20: 66-71. doi: https://doi.org/10.1016/j.bbrc.2022.07.113
3. Corpetti C et al., “Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line,” Phytother. Res. 2021, 35, 12: 6893–6903. doi: https://doi.org/10.1002/ptr.7302
4. Gracie NP et al., “Cellular signalling by SARS-CoV-2 spike protein,” Microbiology Australia 2024, 45, 1: 13-17. doi: https://doi.org/10.1071/MA24005
5. Li F et al., “SARS-CoV-2 Spike Promotes Inflammation and Apoptosis Through Autophagy by ROS-Suppressed PI3K/AKT/mTOR Signaling,” Biochim Biophys Acta BBA – Mol Basis Dis 2021, 1867: 166260. doi: https://doi.org/10.1016/j.bbadis.2021.166260
6. Li K et al., “SARS-CoV-2 Spike protein promotes vWF secretion and thrombosis via endothelial cytoskeleton-associated protein 4 (CKAP4),” Signal Transduct Targ Ther 2022, 7, 332. doi: https://doi.org/10.1038/s41392-022-01183-9
7. Moutal A et al., “SARS-CoV-2 Spike protein co-opts VEGF-A/Neuropilin-1 receptor signaling to induce analgesia,” Pain 2020, 162, 1: 243–252. doi: 10.1097/j.pain.0000000000002097
8. Munavilli GG et al., “COVID-19/SARS-CoV-2 virus spike protein-related delayed inflammatory reaction to hyaluronic acid dermal fillers: a challenging clinical conundrum in diagnosis and treatment,” Arch. Dermatol. Res. 2022, 314: 1-15. doi: https://doi.org/10.1007/s00403-021-02190-6
9. Prieto-Villalobos J et al., “SARS-CoV-2 spike protein S1 activates Cx43 hemichannels and disturbs intracellular Ca2+ dynamics,” Biol Res. 2023, 56, 1: 56. doi: https://doi.org/10.1186/s40659-023-00468-9
10. Rotoli BM et al., “Endothelial cell activation by SARS-CoV-2 spike S1 protein: A crosstalk between endothelium and innate immune cells,” Biomedicines 2021, 9, 9: 1220. doi: https://doi.org/10.3390/biomedicines9091220
11. Singh N and Anuradha Bharara Singh, “S2 Subunit of SARS-nCoV-2 Interacts with Tumor Suppressor Protein p53 and BRCA: An in Silico Study,” Translational Oncology 2020, 13, 10: 100814. doi: https://doi.org/10.1016/j.tranon.2020.100814
12. Singh RD, “The spike protein of sars-cov-2 induces heme oxygenase-1: pathophysiologic implications,” Biochim Biophys Acta, Mol Basis Dis 2022, 1868, 3: 166322. doi: https://doi.org/10.1016/j.bbadis.2021.166322
13. Solis O et al., “The SARS-CoV-2 spike protein binds and modulates estrogen receptors,” Sci. Adv. 2022, 8, 48: eadd4150. doi: 10.1126/sciadv.add4150
14. Suzuki YJ et al., “SARS-CoV-2 spike protein-mediated cell signaling in lung vascular cells,” Vascul. Pharmacol. 2021, 137: 106823. doi: https://doi.org/10.1016/j.vph.2020.106823
15. Suzuki YJ and SG Gychka, “SARS-CoV-2 Spike Protein Elicits Cell Signaling in Human Host Cells: Implications for Possible Consequences of COVID-19 Vaccines,” Vaccines 2021, 9, 1: 36. doi: https://doi.org/10.3390/vaccines9010036
16. Tillman TS et al., “SARS-CoV-2 Spike Protein Downregulates Cell Surface alpha7nAChR through a Helical Motif in the Spike Neck,” ACS Chem. Neurosci. 2023, 14, 4: 689–698. doi: https://doi.org/10.1021/acschemneuro.2c00610
Y. Pregnancy
1. Erdogan MA, “Prenatal SARS-CoV-2 Spike Protein Exposure Induces Autism-Like Neurobehavioral Changes in Male Neonatal Rats,” J Neuroimmune Pharmacol. 2023, 18, 4: 573-591. doi: 10.1007/s11481-023-10089-4
2. Guo X et al., “Regulation of proinflammatory molecules and tissue factor by SARS-CoV-2 spike protein in human placental cells: implications for SARS-CoV-2 pathogenesis in pregnant women,” Front. Immunol. 2022, 13: 876555–876555. doi: https://doi.org/10.3389/fimmu.2022.876555
3. Kammala AK et al., “In vitro mRNA-S maternal vaccination induced altered immune regulation at the maternal-fetal interface,” Am. J. Reprod. Immunol. 2024, 91, 5: e13861. doi: https://doi.org/10.1111/aji.13861
Z. Pulmonary, respiratory
1. Bhargavan B and GD Kanmogne, “SARS-CoV-2 spike proteins and cell–cell communication inhibits TFPI and induces thrombogenic factors in human lung microvascular endothelial cells and neutrophils: implications for COVID-19 coagulopathy pathogenesis,” Int. J. Mol. Sci. 2022, 23, 18: 10436. doi: https://doi.org/10.3390/ijms231810436
2. Biancatelli RMLC et al., “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Kappa18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am. J. Physiol. Lung Cell. Mol. Physiol. 2021, 321: L477–L484. doi: https://doi.org/10.1152/ajplung.00223.2021
3. Cao JB et al., “Mast cell degranulation-triggered by SARS-CoV-2 induces tracheal-bronchial epithelial inflammation and injury,” Virol. Sin. 2024, 39, 2: 309-318. doi: https://doi.org/10.1016/j.virs.2024.03.001
4. Cao X et al., “Spike protein of SARS-CoV-2 activates macrophages and contributes to induction of acute lung inflammation in male mice,” FASEB J. 2021, 35, e21801. doi: https://doi.org/10.1096/fj.202002742RR
5. Caohuy H et al., “Inflammation in the COVID-19 airway is due to inhibition of CFTR signaling by the SARS-CoV-2 spike protein,” Sci. Rep. 2024, 14: 16895. doi: https://doi.org/10.1038/s41598-024-66473-4
6. Chittasupho C et al., “Inhibition of SARS-CoV-2-Induced NLRP3 Inflammasome-Mediated Lung Cell Inflammation by Triphala-Loaded Nanoparticle Targeting Spike Glycoprotein S1,” Pharmaceutics 2024, 16, 6: 751. https://doi.org/10.3390/pharmaceutics16060751
7. Chittasupho C et al., “Targeting spike glycoprotein S1 mediated by NLRP3 inflammasome machinery and the cytokine releases in A549 lung epithelial cells by nanocurcumin,” Pharmaceuticals (Basel) 2023, 16, 6: 862. doi: https://doi.org/10.3390/ph16060862
8. Del Re A et al., “Intranasal delivery of PEA-producing Lactobacillus paracasei F19 alleviates SARS-CoV-2 spike protein-induced lung injury in mice,” Transl. Med. Commun. 2024, 9, 9. doi: https://doi.org/10.1186/s41231-024-00167-x
9. Forsyth CB et al., “The SARS-CoV-2 S1 spike protein promotes MAPK and NF-kB activation in human lung cells and inflammatory cytokine production in human lung and intestinal epithelial cells,” Microorganisms 2022, 10, 10: 1996. doi: https://doi.org/10.3390/microorganisms10101996
10. Greenberger JS et al., “SARS-CoV-2 Spike Protein Induces Oxidative Stress and Senescence in Mouse and Human Lung,” In Vivo 2024, 38, 4: 1546-1556; doi: https://doi.org/10.21873/invivo.13605
11. Jana S et al., “Cell-free hemoglobin does not attenuate the effects of SARS-CoV-2 spike protein S1 subunit in pulmonary endothelial cells,” Int. J. Mol. Sci. 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
12. Kulkoviene G et al., “Differential Mitochondrial, Oxidative Stress and Inflammatory Responses to SARS-CoV-2 Spike Protein Receptor Binding Domain in Human Lung Microvascular, Coronary Artery Endothelial and Bronchial Epithelial Cells,” Int. J. Mol. Sci. 2024, 25, 6: 3188. doi: https://doi.org/10.3390/ijms25063188
13. Liang S et al., “SARS-CoV-2 spike protein induces IL-18-mediated cardiopulmonary inflammation via reduced mitophagy,” Signal Transduct Target Ther 2023, 8, 103. doi: https://doi.org/10.1038/s41392-023-01368-w
14. Liu T et al., “RS-5645 attenuates inflammatory cytokine storm induced by SARS-CoV-2 spike protein and LPS by modulating pulmonary microbiota,” Int J Biol Sci. 2021, 17, 13: 3305–3319. doi: 10.7150/ijbs.63329
15. Palestra F et al. “SARS-CoV-2 Spike Protein Activates Human Lung Macrophages,” Int. J. Mol. Sci. 2023, 24, 3: 3036. doi: https://doi.org/10.3390/ijms24033036
16. Park C et al., “Murine alveolar Macrophages Rapidly Accumulate intranasally Administered SARS-CoV-2 Spike Protein leading to neutrophil Recruitment and Damage,” Elife 2024, 12: RP86764. doi: https://doi.org/10.7554/eLife.86764.3
17. Puthia MTL et al., “Experimental model of pulmonary inflammation induced by SARS-CoV-2 spike protein and endotoxin,” ACS Pharmacol Transl Sci. 2022, 5, 3: 141–8. doi: https://doi.org/10.1021/acsptsci.1c00219
18. Rahman M et al., “Differential Effect of SARS-CoV-2 Spike Glycoprotein 1 on Human Bronchial and Alveolar Lung Mucosa Models: Implications for Pathogenicity,” Viruses 2021, 13, 12: 2537. doi: https://doi.org/10.3390/v13122537
19. Ruben ML et al., “The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells,” Am J Physiol Lung Cell Mol Physiol. 2021, 321, 2: L477-L484. doi: https://doi.org/10.1152/ajplung.00223.2021
20. Segura-Villalobos D et al., “Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein,” Pharmacol. Rep. 2022, 74: 1315–1325. doi: https://doi.org/10.1007/s43440-022-00398-5
21. Semmarath W et al., “Cyanidin-3-O-glucoside and Peonidin-3-O-glucoside-Rich Fraction of Black Rice Germ and Bran Suppresses Inflammatory Responses from SARS-CoV-2 Spike Glycoprotein S1-Induction In Vitro in A549 Lung Cells and THP-1 Macrophages via Inhibition of the NLRP3 Inflammasome Pathway,” Nutrients 2022, 14, 13: 2738. doi: https://doi.org/10.3390/nu14132738
22. Sirsendu J et al., “Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells,” Int. J. Mol. Sci. 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
23. Sui Y et al., “SARS-CoV-2 Spike Protein Suppresses ACE2 and Type I Interferon Expression in Primary Cells From Macaque Lung Bronchoalveolar Lavage,” Front. Immunol. 2021, 12. doi: https://doi.org/10.3389/fimmu.2021.658428
24. Sung PS et al., “CLEC5A and TLR2 Are Critical in SARS-CoV-2-Induced NET Formation and Lung Inflammation,” J. Biomed. Sci. 2022, 29, 52. doi: https://doi.org/10.1186/s12929-022-00832-z
25. Suzuki YJ et al., “SARS-CoV-2 spike protein-mediated cell signaling in lung vascular cells,” Vascul. Pharmacol. 2021, 137: 106823. doi: https://doi.org/10.1016/j.vph.2020.106823
26. Zekri-Nechar K et al., “Spike Protein Subunits of SARS-CoV-2 Alter Mitochondrial Metabolism in Human Pulmonary Microvascular Endothelial Cells: Involvement of Factor Xa,” Dis. Markers 2022, 1118195. doi: https://doi.org/10.1155/2022/1118195
AA. Renin-Angiotensin-Aldosterone System
1. Lehmann KJ, “SARS-CoV-2-Spike Interactions with the Renin-Angiotensin-Aldosterone System – Consequences of Adverse Reactions of Vaccination,” J Biol Today’s World 2023, 12/4: 001-013. doi: https://doi.org/10.31219/osf.io/27g5h
2. Matsuzawa Y et al., “Impact of Renin–Angiotensin–Aldosterone System Inhibitors on COVID-19,” Hypertens. Res. 2022, 45, 7: 1147–1153, doi: https://doi.org/10.1038/s41440-022-00922-3
BB. Senescence/aging
1. Duarte C, “Age-dependent effects of the recombinant spike protein/SARS-CoV-2 on the M-CSF- and IL-34-differentiated macrophages in vitro,” Biochem. Biophys. Res. Commun. 2021, 546: 97–102. doi: https://doi.org/10.1016/j.bbrc.2021.01.104
2. Greenberger JS et al., “SARS-CoV-2 Spike Protein Induces Oxidative Stress and Senescence in Mouse and Human Lung,” In Vivo 2024, 38, 4: 1546-1556. doi: https://doi.org/10.21873/invivo.13605
3. Meyer K et al., “SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells,” J. Virol. 2021, 95, e0079421. doi: https://doi.org/10.1128/jvi.00794-21
CC. Stem cells
1. Balzanelli MG et al., “The Role of SARS-CoV-2 Spike Protein in Long-term Damage of Tissues and Organs, the Underestimated Role of Retrotransposons and Stem Cells, a Working Hypothesis,” Endocr Metab Immune Disord Drug Targets 2025, 25, 2: 85-98. doi: 10.2174/0118715303283480240227113401
2. Kucia M et al. “An evidence that SARS-Cov-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner,” Leukemia 2021, 35: 3026-3029. doi: https://doi.org/10.1038/s41375-021-01332-z
3. Ropa J et al., “Human Hematopoietic Stem, Progenitor, and Immune Cells Respond Ex Vivo to SARS-CoV-2 Spike Protein,” Stem Cell Rev Rep. 2021, 17, 1: 253-265. doi: https://doi.org/10.1007/s12015-020-10056-z
DD. Syncytia/cell fusion
1. Braga L et al., “Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia,” Nature 2021, 594: 88–93. doi: https://doi.org/10.1038/s41586-021-03491-6
2. Cattin‐Ortolá J et al., “Sequences in the cytoplasmic tail of SARS‐CoV‐2 Spike facilitate expression at the cell surface and syncytia formation,” Nat Commun 2021, 12, 1: 5333. doi: https://doi.org/10.1038/s41467-021-25589-1
3. Clemens DJ et al., “SARS-CoV-2 spike protein-mediated cardiomyocyte fusion may contribute to increased arrhythmic risk in COVID-19,” PLoS One 2023, 18, 3: e0282151. doi: https://doi.org/10.1371/journal.pone.0282151
4. Lazebnik Y, “Cell fusion as a link between the SARS-CoV-2 spike protein, COVID-19 complications, and vaccine side effects,” Oncotarget 2021, 12, 25: 2476-2488. doi: https://doi.org/10.18632/oncotarget.28088
5. Liu X et al., “SARS-CoV-2 spike protein-induced cell fusion activates the cGAS-STING pathway and the interferon response,” Sci Signal. 2022, 15, 729: eabg8744. doi: 10.1126/scisignal.abg8744
6. Martinez-Marmol R et al., “SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity,” Sci. Adv. 2023, 9, 23. doi: 10.1126/sciadv.adg2248
7. Rajah MM et al., “SARS-CoV-2 Alpha, Beta, and Delta variants display enhanced spike-mediated syncytia formation,” EMBO J. 2021, 40: e108944. doi: https://doi.org/10.15252/embj.2021108944
8. Shirato K and Takako Kizaki, “SARS-CoV-2 Spike Protein S1 Subunit Induces Pro- inflammatory Responses via Toll-Like Receptor 4 Signaling in Murine and Human Macrophages,” Heliyon 2021, 7, 2: e06187. doi: https://doi.org/10.1016/j.heliyon.2021.e06187
9. Theuerkauf SA et al., “Quantitative assays reveal cell fusion at minimal levels of SARS-CoV-2 spike protein and fusion from without,” iScience 2021, 24, 3: 102170. doi: https://doi.org/10.1016/j.isci.2021.102170
10. Zhang Z et al., “SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination,” Cell Death Differ. 2021, 28: 2765–2777. doi: https://doi.org/10.1038/s41418-021-00782-3
EE. Therapeutics
1. Almehdi AM et al., “SARS-CoV-2 Spike Protein: Pathogenesis, Vaccines, and Potential Therapies,” Infection 2021, 49, 5: 855–876. doi: https://doi.org/10.1007/s15010-021-01677-8
2. Boretti A, “PQQ Supplementation and SARS-CoV-2 Spike Protein-Induced Heart Inflammation,” Nat. Prod. Commun. 2022, 17, 1934578×221080929. doi: https://doi.org/10.1177/1934578X221080929
3. Boschi C et al., “SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects,” Int. J. Biol. Macromol. 2022, 23, 24: 15480. doi: https://doi.org/10.3390/ijms232415480
4. Braga L et al., “Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia,” Nature 2021, 594: 88–93. doi: https://doi.org/10.1038/s41586-021-03491-6
5. Chang MH et al., “SARS-CoV-2 Spike Protein 1 Causes Aggregation of α-Synuclein via Microglia-Induced Inflammation and Production of Mitochondrial ROS: Potential Therapeutic Applications of Metformin,” Biomedicines 2024, 12, 6: 1223. doi: https://doi.org/10.3390/biomedicines12061223
6. Chittasupho C et al., “Inhibition of SARS-CoV-2-Induced NLRP3 Inflammasome-Mediated Lung Cell Inflammation by Triphala-Loaded Nanoparticle Targeting Spike Glycoprotein S1,” Pharmaceutics 2024, 16, 6: 751. doi: https://doi.org/10.3390/pharmaceutics16060751
7. Chittasupho C et al., “Targeting spike glycoprotein S1 mediated by NLRP3 inflammasome machinery and the cytokine releases in A549 lung epithelial cells by nanocurcumin,” Pharmaceuticals (Basel) 2023, 16, 6: 862. doi: https://doi.org/10.3390/ph16060862
8. Corpetti C et al., “Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line,” Phytother. Res. 2021, 35, 12: 6893–6903. doi: https://doi.org/10.1002/ptr.7302
9. Cory TJ et al., “Metformin Suppresses Monocyte Immunometabolic Activation by SARS-CoV-2 Spike Protein Subunit 1,” Front. Immunol. 2021, 12 (Sec. Cytokines and Soluble Mediators in Immunity): 733921. doi: https://doi.org/10.3389/fimmu.2021.733921
10. Del Re A et al., “Intranasal delivery of PEA-producing Lactobacillus paracasei F19 alleviates SARS-CoV-2 spike protein-induced lung injury in mice,” Transl. Med. Commun. 2024, 9, 9. doi: https://doi.org/10.1186/s41231-024-00167-x
11. Del Re A et al., “Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages,” Metabolites 2021, 11, 9: 592. doi: https://doi.org/10.3390/metabo11090592
12. Ferrer MD et al., “Nitrite Attenuates the In Vitro Inflammatory Response of Immune Cells to the SARS-CoV-2 S Protein without Interfering in the Antioxidant Enzyme Activation,” Int. J. Mol. Sci. 2024, 25, 5: 3001. https://doi.org/10.3390/ijms25053001
13. Frank MG et al., “SARS-CoV-2 S1 subunit produces a protracted priming of the neuroinflammatory, physiological, and behavioral responses to a remote immune challenge: A role for corticosteroids,” Brain Behav. Immun. 2024, 121: 87-103. doi: https://doi.org/10.1016/j.bbi.2024.07.034
14. Frühbeck G et al., “FNDC4 and FNDC5 reduce SARS-CoV-2 entry points and spike glycoprotein S1-induced pyroptosis, apoptosis, and necroptosis in human adipocytes,” Cell Mol Immunol. 2021, 18, 10: 2457–9. doi: https://doi.org/10.1038/s41423-021-00762-0
15. Gasparello J et al., “Sulforaphane inhibits the expression of interleukin-6 and interleukin-8 induced in bronchial epithelial IB3-1 cells by exposure to the SARS-CoV-2 Spike protein,” Phytomedicine 2021, 87: 153583. doi: https://doi.org/10.1016/j.phymed.2021.153583
16. Halma MTJ et al., “Exploring autophagy in treating SARS-CoV-2 spike protein-related pathology,” Endocrinol Metab (EnM) 2024, 14: 100163. doi: https://doi.org/10.1016/j.endmts.2024.100163
17. Halma MTJ et al., “Strategies for the Management of Spike Protein-Related Pathology,” Microorganisms 2023, 11, 5: 1308. doi: https://doi.org/10.3390/microorganisms11051308
18. Jana S et al., “Cell-free hemoglobin does not attenuate the effects of SARS-CoV-2 spike protein S1 subunit in pulmonary endothelial cells,” Int. J. Mol. Sci. 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
19. Jugler C et al., “SARS-CoV-2 Spike Protein-Induced Interleukin 6 Signaling Is Blocked by a Plant-Produced Anti-Interleukin 6 Receptor Monoclonal Antibody,” Vaccines 2021, 9, 11: 1365. doi: https://doi.org/10.3390/vaccines9111365
20. Ken W et al., “Low dose radiation therapy attenuates ACE2 depression and inflammatory cytokines induction by COVID-19 viral spike protein in human bronchial epithelial cells,” Int J Radiat Biol. 2022, 98, 10:1532-1541. doi: https://doi.org/10.1080/09553002.2022.2055806
21. Kumar N et al., “SARS-CoV-2 spike protein S1-mediated endothelial injury and pro-inflammatory state Is amplified by dihydrotestosterone and prevented by mineralocorticoid antagonism,” Viruses 2021, 13, 11: 2209. doi: https://doi.org/10.3390/v13112209
22. Liu T et al., “RS-5645 attenuates inflammatory cytokine storm induced by SARS-CoV-2 spike protein and LPS by modulating pulmonary microbiota,” Int J Biol Sci. 2021, 17, 13: 3305–3319. doi: 10.7150/ijbs.63329
23. Loh D, “The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding,” Melatonin Research 2020, 3, 3: 380-416. doi: https://doi.org/10.32794/mr11250069
24. Loh JT et al., “Dok3 restrains neutrophil production of calprotectin during TLR4 sensing of SARS-CoV-2 spike protein,” Front. Immunol. 2022, 13 (Sec. Molecular Innate Immunity). doi: https://doi.org/10.3389/fimmu.2022.996637
25. Marrone L et al., “Tirofiban prevents the effects of SARS-CoV-2 spike protein on macrophage activation and endothelial cell death,” Heliyon 2024, 10, 15: e35341. doi: 10.1016/j.heliyon.2024.e35341
26. Norris B et al., “Evaluation of Glutathione in Spike Protein of SARS-CoV-2 Induced Immunothrombosis and Cytokine Dysregulation,” Antioxidants 2024, 13, 3: 271. doi: https://doi.org/10.3390/antiox13030271
27. Olajide OA et al., “Induction of Exaggerated Cytokine Production in Human Peripheral Blood Mononuclear Cells by a Recombinant SARS-CoV-2 Spike Glycoprotein S1 and Its Inhibition by Dexamethasone,” Inflammation 2021, 44: 1865–1877. doi: https://doi.org/10.1007/s10753-021-01464-5
28. Petrosino S and N Matende, “Elimination/Neutralization of COVID-19 Vaccine-Produced Spike Protein: Scoping Review,” Mathews Journal of Nutrition & Dietetics 2024, 7, 2. doi: https://doi.org/10.30654/MJND.10034
29. Satta S et al., “An engineered nano-liposome-human ACE2 decoy neutralizes SARS-CoV-2 Spike protein-induced inflammation in both murine and human macrophages,” Theranostics 2022, 12, 6: 2639–2657. doi: 10.7150/thno.66831
30. Segura-Villalobos D et al., “Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein,” Pharmacol. Rep. 2022, 74: 1315–1325. doi: https://doi.org/10.1007/s43440-022-00398-5
31. Semmarath W et al., “Cyanidin-3-O-glucoside and Peonidin-3-O-glucoside-Rich Fraction of Black Rice Germ and Bran Suppresses Inflammatory Responses from SARS-CoV-2 Spike Glycoprotein S1-Induction In Vitro in A549 Lung Cells and THP-1 Macrophages via Inhibition of the NLRP3 Inflammasome Pathway,” Nutrients 2022, 14, 13: 2738. doi: https://doi.org/10.3390/nu14132738
32. Suprewicz L et al., “Recombinant human plasma gelsolin reverses increased permeability of the blood-brain barrier induced by the spike protein of the SARS-CoV-2 virus,” J Neuroinflammation 2022, 19, 1: 282. doi: https://doi.org/10.1186/s12974-022-02642-4
33. Vargas-Castro R et al., “Calcitriol prevents SARS-CoV spike-induced inflammation in human trophoblasts through downregulating ACE2 and TMPRSS2 expression,” J Steroid Biochem Mol Biol 2025, 245: 106625. doi: https://doi.org/10.1016/j.jsbmb.2024.106625
34. Youn JY et al., “Therapeutic application of estrogen for COVID-19: Attenuation of SARS-CoV-2 spike protein and IL-6 stimulated, ACE2-dependent NOX2 activation, ROS production and MCP-1 upregulation in endothelial cells,” Redox Biol. 2021, 46: 102099. doi: https://doi.org/10.1016/j.redox.2021.102099
35. Yu J et al., “Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition,” Blood 2020, 136, 18: 2080–2089. doi: https://doi.org/10.1182/blood.2020008248
FF. Toll-like receptors (TLRs)
1. Aboudounya MM and RJ Heads, “COVID-19 and Toll-Like Receptor 4 (TLR4): SARS-CoV-2 May Bind and Activate TLR4 to Increase ACE2 Expression, Facilitating Entry and Causing Hyperinflammation,” Mediators Inflamm. 2021: 8874339. doi: https://doi.org/10.1155/2021/8874339
2. Burnett FN et al., “SARS-CoV-2 Spike Protein Intensifies Cerebrovascular Complications in Diabetic hACE2 Mice through RAAS and TLR Signaling Activation,” Int. J. Mol. Sci. 2023, 24, 22: 16394. doi: https://doi.org/10.3390/ijms242216394
3. Carnevale R et al., “Toll-Like Receptor 4-Dependent Platelet-Related Thrombosis in SARS-CoV-2 Infection,” Circ. Res. 2023, 132, 3: 290– 305. doi: https://doi.org/10.1161/CIRCRESAHA.122.321541
4. Corpetti C et al., “Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line,” Phytother. Res. 2021, 35, 12: 6893–6903. doi: https://doi.org/10.1002/ptr.7302
5. Fontes-Dantas FL, “SARS-CoV-2 Spike Protein Induces TLR4-Mediated Long- Term Cognitive Dysfunction Recapitulating Post-COVID-19 Syndrome in Mice,” Cell Reports 2023, 42, 3: 112189, doi: https://doi.org/10.1016/j.celrep.2023.112189
6. Khan S et al., “SARS-CoV-2 Spike Protein Induces Inflammation via TLR2-Dependent Activation of the NF-κB Pathway,” eLife 2021, 10: e68563. doi: https://doi.org/10.7554/elife.68563
7. Kim MJ et al., “The SARS‐CoV‐2 spike protein induces lung cancer migration and invasion in a TLR2‐dependent manner,” Cancer Commun (London) 2023, 44, 2: 273–277. doi: https://doi.org/10.1002/cac2.12485
8. Kircheis R and O Planz, “Could a Lower Toll-like Receptor (TLR) and NF-κB Activation Due to a Changed Charge Distribution in the Spike Protein Be the Reason for the Lower Pathogenicity of Omicron?” Int. J. Mol. Sci. 2022, 23, 11: 5966. doi: https://doi.org/10.3390/ijms23115966
9. Loh JT et al., “Dok3 restrains neutrophil production of calprotectin during TLR4 sensing of SARS-CoV-2 spike protein,” Front. Immunol. 2022, 13 (Sec. Molecular Innate Immunity). doi: https://doi.org/10.3389/fimmu.2022.996637
10. Segura-Villalobos D et al., “Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein,” Pharmacol. Rep. 2022, 74: 1315–1325. doi: https://doi.org/10.1007/s43440-022-00398-5
11. Sirsendu J et al., “Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells,” Int. J. Mol. Sci., 2021, 22, 16: 9041. doi: https://doi.org/10.3390/ijms22169041
12. Sung PS et al., “CLEC5A and TLR2 Are Critical in SARS-CoV-2-Induced NET Formation and Lung Inflammation,” J. Biomed. Sci. 2022, 29, 52. doi: https://doi.org/10.1186/s12929-022-00832-z
13. Zaki H and S Khan, “SARS-CoV-2 spike protein induces inflammatory molecules through TLR2 in macrophages and monocytes,” J. Immunol. 2021, 206 (1_supplement): 62.07. doi: https://doi.org/10.4049/jimmunol.206.Supp.62.07
14. Zaki H and S Khan, “TLR2 senses spike protein of SARS-CoV-2 to trigger inflammation,” J. Immunol. 2022, 208 (1_Supplement): 125.30. doi: https://doi.org/10.4049/jimmunol.208.Supp.125.30
15. Zhao Y et al., “SARS-CoV-2 spike protein interacts with and activates TLR4,” Cell Res. 2021, 31: 818–820. doi: https://doi.org/10.1038/s41422-021-00495-9
___
You must not wait for another catastrophic crisis (at times manufactured but we are prevented from making our own basic personal decisions or accessing needed drugs and response tools) to catch you off-guard. We must take charge and be prepared today so that we can enjoy peace of mind tomorrow.
Enter the Wellness Company as a solution and a willing participant in the health care conversation. From telemedicine, prescriptions, memberships, and supplements, TWC is leading America with alternative choices to the traditional health care model.
If you wish to give a donation to help me, you can at:
Zelle:
sr7283@gmail.com
Or Ko-Fi
Ko-fi.com/drpauleliasalexander
Or to my address at:
150 South 8th Street
Unit 170
Lewiston, New York
14092
Alternatively, please consider going from an UNPAID subscriber or follower to a PAID at $5 per month or $30 per year. This can provide me help. If this is not possible at this time, this is ok, please remain a subscriber for FREE and there is no difference between FREE and PAID. No restrictions.
Please consider support of a good PATRIOT company (in this PATRIOT economy) Drs. McCullough, Risch, Thorp, myself support (they are our sponsors), The Wellness Company; see the emergency preparation kit (key component being antibiotics you were denied by doctors, pharmacists, governments during the fraud COVID), first aid kit, travel emergency kit, contagion control kit etc. Please consider the SPIKE SUPPORT (spike protein DETOX dissolving spike from mRNA vaccine, this is critical to remove spike form the mRNA vaccine/and DNA viral vector) formula with NATTOKINASE as well as the triple formula (SPIKE SUPPORT, BROMELAIN, CIRCUMIN)
Discussion about this post








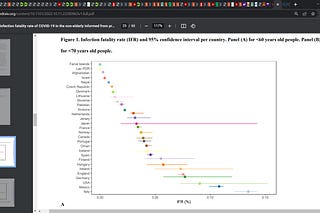

May 21, 2022
It’s interesting to me that it’s people in their 40s or younger that haven’t had the smallpox vaccine.
I wonder if this story will end with with the younger age brackets being urged to take a new vax because they’re at greater risk?
It would be a great way to mop up the age bands with lowest uptake of Covid jabs. Not that I’m cynical or anything.
May 21, 2022
The Smallpox Pandemic Response was Eerily Similar to COVID – Quackcines killing more people than the disease!!!
https://amidwesterndoctor.substack.com/p/the-smallpox-pandemic-response-was?s=w